When your Achilles or kneecap tendon starts hurting during a run, a jump, or even just walking up stairs, it’s not just soreness-it’s tendinopathy. This isn’t a simple inflammation. It’s a degenerative breakdown of tendon tissue, often caused by repeated stress without enough recovery. You might have tried rest, ice, or a cortisone shot, but those rarely fix the root problem. The real solution? A proven, science-backed approach: eccentric training. And when that’s not enough, injections can play a role-but not always the way you think.
What Exactly Is Tendinopathy?
Tendinopathy happens when the tendon, the strong band connecting muscle to bone, starts to break down. It’s not swelling like a sprain. It’s more like fraying rope. The collagen fibers inside the tendon get disorganized, lose their strength, and start to hurt. You’ll feel pain during activity, stiffness in the morning, and sometimes a lump or thickening in the tendon itself. The most common sites? The Achilles (back of the ankle) and patellar tendon (just below the kneecap). But it can hit the shoulder, elbow, or even the hip.
It’s not just athletes. A 45-year-old who suddenly started gardening, a nurse on their feet all day, or a weekend basketball player can all develop it. Studies show about 30% of sports medicine visits involve tendinopathy. And here’s the catch: rest alone doesn’t fix it. In fact, avoiding movement often makes the tendon weaker over time.
Eccentric Training: The Gold Standard
In 1998, Dr. Hakan Alfredson published a simple but radical idea: instead of avoiding pain, use controlled, slow lowering movements to rebuild the tendon. That’s eccentric training. It’s not about lifting heavy. It’s about controlling the descent.
For Achilles tendinopathy, the classic protocol is the Alfredson heel drop. You stand on the edge of a step, raise up on both feet, then slowly lower the injured foot down over 3-5 seconds. Do 3 sets of 15 reps, twice a day, with your knee straight (targets the calf muscle) and bent (targets the deeper soleus). You’ll feel it. Pain during the exercise is normal, even expected. But if it spikes past a 7/10 or lasts more than 24 hours, you’re pushing too hard.
For patellar tendinopathy, it’s single-leg decline squats. You stand on a 25-degree angled board (or a thick book under your toes), and slowly lower into a squat over 3-5 seconds. Again, 3 sets of 15, daily. The decline increases the load on the patellar tendon, forcing it to adapt.
These aren’t quick fixes. You need 12 weeks of consistent effort. Ultrasound scans show real changes after 8-12 weeks: the tendon thickens in a healthy way, collagen fibers realign, and stiffness increases by 15-20%. That’s not just less pain-it’s a stronger, more resilient tendon.
Heavy Slow Resistance: The Alternative That Works Just as Well
Not everyone can handle the high pain load of eccentric heel drops. That’s where heavy slow resistance (HSR) comes in. Instead of doing 15 reps with bodyweight, you use a weight-around 70% of your one-rep max-and do 3 sets of 15 reps, three times a week.
Here’s the surprising part: a 2015 study in the Journal of Orthopaedic & Sports Physical Therapy found HSR improved Achilles tendinopathy just as much as eccentric training. Both groups saw a 60-65% improvement in VISA-A scores. But HSR had one big advantage: better adherence. 87% stuck with it. Only 72% stuck with eccentric training. Why? Less initial pain. You’re not dropping your heel into agony-you’re lifting and lowering with control.
HSR works for patellar tendinopathy too. Squatting with a barbell or machine, slow and controlled, builds tendon strength without the extreme discomfort. It’s a great option if you’ve tried eccentric training and quit because it was too painful.

Isometric Exercises: The Pain Relief Trick
Need to get through a workout or walk without agony? Try isometrics. These are static holds-no movement. For the Achilles, stand on your toes and hold the position for 45 seconds. For the patellar tendon, do a wall sit with knees at 90 degrees and hold.
A 2015 study showed isometrics reduce pain by 50% within 45 minutes. That’s faster than any injection. It doesn’t rebuild the tendon long-term, but it’s a powerful tool to manage pain before activity. Use it as a warm-up or cooldown. It can help you stay active while your tendon heals.
Injections: What Actually Works (and What Doesn’t)
Let’s talk about injections. Cortisone shots are common. They feel great at first-pain drops 30-50% in 2-4 weeks. But here’s the catch: a 2013 BMJ study found that 65% of people who got cortisone needed more treatment within 6 months. The tendon didn’t heal. It just got numb. And repeated shots can weaken the tendon further.
Platelet-rich plasma (PRP) is another popular option. It sounds fancy-your own blood, spun to concentrate healing cells. But a 2020 review in the American Journal of Sports Medicine found PRP only beat placebo by 15-20% at 6 months. Not enough to justify the cost, especially when exercise has proven results.
So what’s the verdict? Injections aren’t the answer. They’re a temporary band-aid. Eccentric training, HSR, and isometrics are the real treatment. Use injections only if you’re stuck, in severe pain, and need a short-term reset to start exercising again.
Why Most People Fail (and How to Succeed)
Here’s the hard truth: 30% of people don’t respond to eccentric training. Why? Three reasons.
- They quit too early. You need 12 weeks. Most give up by week 4 because it still hurts.
- They do it wrong. A 2021 study found self-managed patients made technique errors 40% of the time. If your knee caves inward during a decline squat, you’re not loading the tendon correctly.
- They ignore pain signals. Pain between 2-5/10 during exercise? Acceptable. Pain over 7/10? Stop. Pain lasting over 24 hours? You overdid it. Only 38% of self-managed patients understand this.
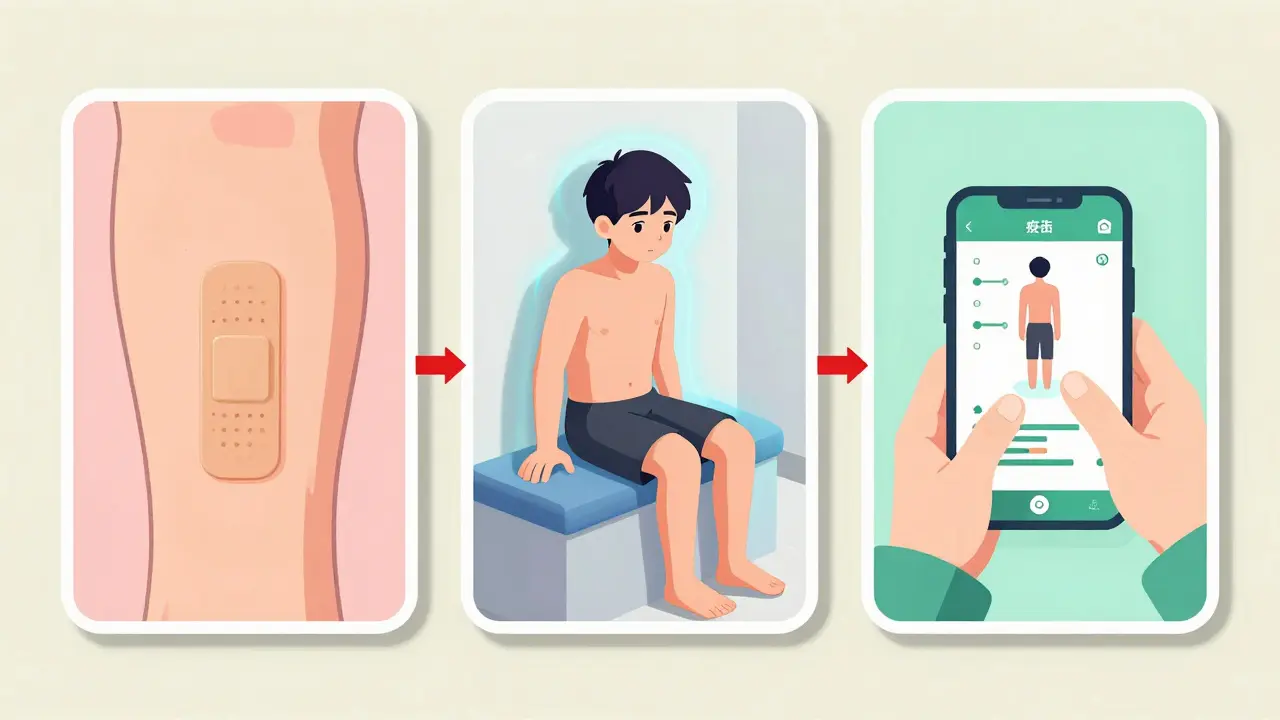
Success comes from consistency, not intensity. Use a tracking app like Tendon Rehab (version 3.2, 2023). It gives feedback, reminds you, and logs your pain levels. People using apps had 85% adherence. Paper plans? Only 65%.
And work with a physical therapist-even once. Get your form checked. It cuts failure rates in half.
The Bigger Picture: Load Management Matters Too
Dr. Neal Barton points out a blind spot: we focus so much on exercise that we forget about daily load. If you’re a runner with Achilles tendinopathy but still hike 10 miles on weekends, you’re undoing your rehab. Tendons need balance-not just strengthening, but smart loading.
That means adjusting your activity. Reduce high-impact tasks. Swap running for cycling or swimming. Build up slowly. Recovery isn’t passive. It’s active planning.
What’s Next for Tendinopathy Treatment?
The future isn’t just about exercises. Researchers are moving toward “precision rehabilitation.” Think blood tests or ultrasound scans that show exactly where your tendon is in its healing process. A 2022 study found tailoring load based on individual tendon response improved outcomes by 25%.
Early trials are testing peptides that activate tendon cells. These aren’t available yet, but they hint at a future where treatment is personalized, not one-size-fits-all.
For now, the best option remains clear: controlled, consistent movement. Eccentric training. Heavy slow resistance. Isometrics. And patience. No magic shot. No quick fix. Just time, effort, and the right plan.
How long does it take to see results from eccentric training for tendinopathy?
You’ll start noticing less pain after 4-6 weeks, but real structural changes take 8-12 weeks. Ultrasound scans show improved tendon texture and thickness by week 12. Most people need the full 12 weeks to return to full activity without pain. Don’t rush it-tendons heal slowly.
Is eccentric training painful? Should I stop if it hurts?
Yes, it’s often painful at first-68% of patients report high pain in the first two weeks. But pain between 2 and 5 out of 10 during exercise is normal and expected. It should go away within 24 hours. If pain is over 7/10, or lasts longer than a day, you’re overdoing it. Back off slightly. Pain is a signal, not a failure.
Can I do eccentric training at home without a therapist?
Yes, many people do. But a single session with a physical therapist to check your form cuts your risk of failure in half. Mistakes like knee collapse during decline squats or improper heel drop angle reduce effectiveness. Use video tutorials or apps like Tendon Rehab to self-correct. If you’ve tried and failed before, a professional check-up is worth it.
Are cortisone injections a good option for tendinopathy?
They offer short-term relief-30-50% pain reduction in 4 weeks-but they don’t fix the tendon. A 2013 study found 65% of people needed more treatment within 6 months. Repeated injections can weaken the tendon. Use them only as a last resort to get you through a critical period so you can start exercise. They’re not a cure.
What’s the difference between eccentric training and heavy slow resistance?
Eccentric training focuses on slow lowering (eccentric phase) using bodyweight, like heel drops or decline squats. Heavy slow resistance (HSR) uses weights-around 70% of your max-and controls both the lifting (concentric) and lowering phases. Both rebuild tendons. HSR is often easier to stick with because it’s less painful at first. Choose based on your pain tolerance and access to equipment.
Can I still run or play sports while doing eccentric training?
Yes, but you need to modify. Reduce high-impact activities. Swap some runs for cycling or swimming. Don’t push through sharp pain. Use isometric holds before activity to manage pain. The goal is to keep moving without overloading the tendon. Most people who complete 12 weeks of training return to their previous activity levels-82% of runners in one survey did.


Tendinopathy isn't some trendy fitness buzzword-it's a slow-motion disaster waiting to happen. I tried eccentric training for my Achilles. Week one: fine. Week two: I cried. Week three: I swore off exercise forever. But guess what? Week twelve? I ran a 5K without wincing. No magic shot. No miracle cure. Just pain, persistence, and a damn spreadsheet tracking my pain levels. If you're not ready to suffer, don't bother.