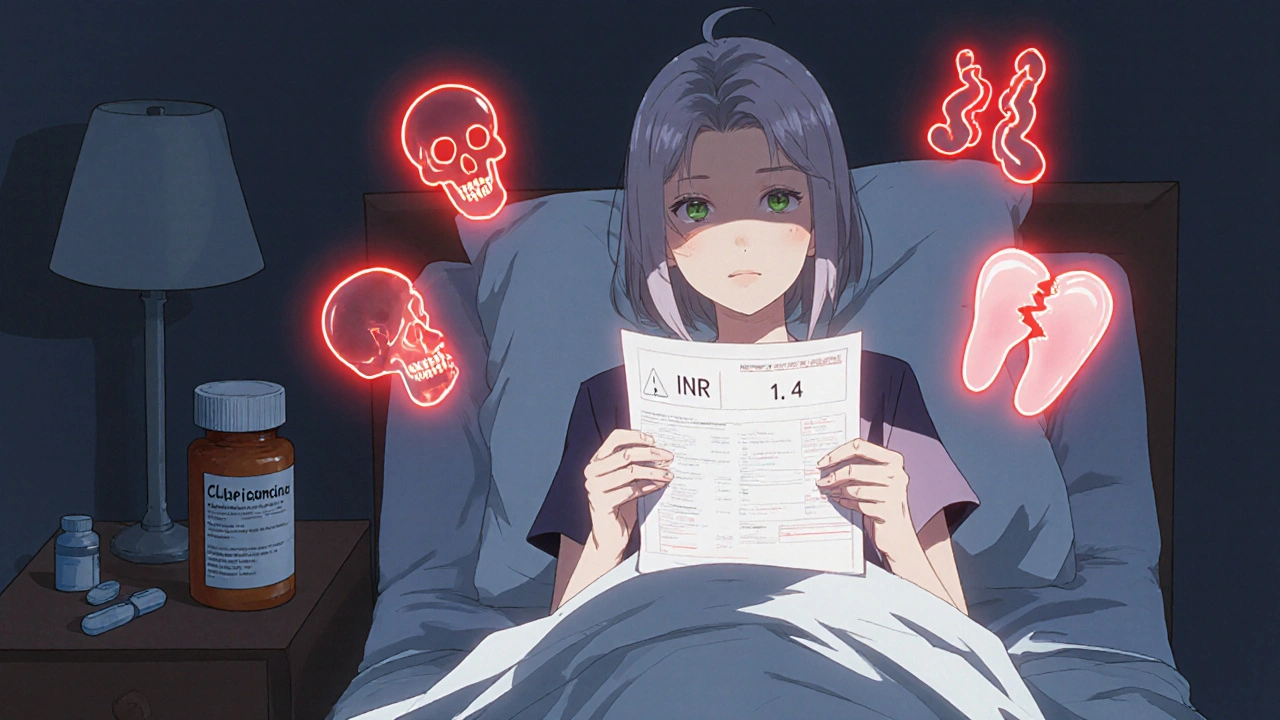
Warfarin Antibiotic Risk Calculator
Calculate Your Antibiotic Risk
Enter your antibiotic choice and health factors to see INR risk level and recommended actions.
Results will appear here after calculation
When you're on warfarin, even a simple antibiotic for a sinus infection or urinary tract infection can throw your blood thinning off balance - sometimes dangerously so. You might not realize it until you start bleeding for no reason, or worse, end up in the hospital. This isn't rare. Every year, thousands of people on warfarin experience dangerous spikes in their INR because of antibiotics they took without knowing the risk.
Why Warfarin Is So Sensitive
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It’s a tightrope walk: too little, and you risk clots; too much, and you bleed. Your INR tells you where you stand. For most people, the safe range is 2.0 to 3.0. Once it hits 5.0 or higher, your risk of internal bleeding - in the brain, gut, or elsewhere - jumps sharply.
What makes warfarin so tricky is how your body processes it. About 90% of it is broken down by liver enzymes called CYP2C9 and CYP3A4. Many antibiotics interfere with these enzymes. Some block them, making warfarin stick around longer. Others kill off the good bacteria in your gut that make vitamin K - cutting your natural counterbalance to warfarin. Both pathways push your INR up, often without warning.
Not All Antibiotics Are Equal
Some antibiotics barely touch your INR. Others? They’re ticking time bombs.
High-risk antibiotics that commonly spike INR:
- Fluoroquinolones - levofloxacin and ciprofloxacin. Even though some studies say ciprofloxacin is low risk, others show levofloxacin raises INR by 2 to 4 points in over 20% of users. Bleeding risk triples compared to warfarin alone.
- Macrolides - clarithromycin is dangerous. It can raise INR by 1.8 to 2.5 points in nearly one-third of patients. Azithromycin? Almost no effect. The difference matters.
- Sulfonamides - trimethoprim-sulfamethoxazole (Bactrim) is a double threat. It inhibits CYP2C9 and kills vitamin K-producing bacteria. INR spikes of 1.2 to 3.0 are common within 4 to 7 days.
- Metronidazole - used for vaginal infections or dental abscesses. It boosts INR by 1.5 to 2.8 points in about one in three people. The effect peaks around day 7 to 10.
Low-risk antibiotics - these usually don’t cause problems:
- Penicillins (amoxicillin, ampicillin)
- Cephalosporins (cefazolin, ceftriaxone)
Even with low-risk options, exceptions happen. One person might have a rare reaction. That’s why you never assume - you check.
The Delay Is the Danger
The biggest mistake people make? Thinking if they feel fine, their INR is fine. But here’s the catch: the biggest INR spikes don’t show up right away.
When antibiotics kill gut bacteria that make vitamin K, it takes 3 to 7 days for vitamin K levels to drop enough to affect clotting. So if you start an antibiotic on Monday, your INR might stay normal until Thursday or Friday. By then, you’re already in the danger zone.
And when you stop the antibiotic? Your gut bacteria start recovering. Vitamin K production bounces back. Your INR can drop fast - sometimes from 2.8 down to 1.1 in just 3 days. That’s not just under-thinning; that’s stroke risk.

Who’s Most at Risk?
Not everyone reacts the same. Certain people are far more likely to have a bad reaction:
- Age 75+ - metabolism slows, kidneys don’t clear drugs as well.
- Baseline INR above 2.5 - you’re already close to the edge.
- Cancer patients - disease and treatments alter drug processing.
- Women - studies show a 42% higher risk of dangerous INR spikes compared to men.
If you fit any of these, even a low-risk antibiotic needs extra caution.
What You Should Do - Step by Step
If you’re on warfarin and your doctor prescribes an antibiotic:
- Ask: Is this antibiotic high-risk? Don’t assume it’s safe. Ask for the name and check if it’s on the high-risk list.
- Get your INR checked 3 to 5 days after starting the antibiotic. Even if you feel fine. Don’t wait for symptoms.
- Check again 7 to 10 days after stopping the antibiotic. Your INR can crash as your gut bacteria recover.
- Don’t change your warfarin dose yourself. Your doctor will adjust based on your INR. If your INR is above 5.0, you may need vitamin K or even hospitalization.
- Keep a log. Write down every antibiotic you take, the date you started and stopped, and your INR results. Bring it to every appointment.

Real Stories, Real Consequences
In 2022, a 78-year-old man in Melbourne was prescribed amoxicillin for a cough. He didn’t think it mattered. His INR was stable at 2.3. Three days later, he fell and hit his head. He woke up in the ER with a brain bleed. His INR was 8.9. The amoxicillin wasn’t the direct cause - but his doctor never checked his INR after starting it. He’d been on warfarin for 12 years. He survived, but he lost his independence.
Another case: a woman in her 60s took clarithromycin for bronchitis. Her INR jumped from 2.7 to 11.4 in 6 days. She started bleeding from her gums and nose. She needed vitamin K and a hospital stay. Her pharmacist had warned her, but she didn’t believe it could happen to her.
These aren’t outliers. A 2021 study found that nearly a quarter of warfarin-related ER visits involved recent antibiotic use. Over 60% of those cases had INR above 5.0.
What’s New in 2025
Technology is helping. New home INR monitors - like the Roche CoaguChek INRange - connect to your phone. You can test your INR daily while on antibiotics and send results to your doctor instantly. Some clinics now use AI tools that predict how your INR will react based on your genetics, age, meds, and even your diet.
But tech won’t fix bad habits. A 2023 CDC survey found that over one-third of warfarin users were given antibiotics they didn’t even need. Unnecessary prescriptions are still the biggest risk.
Bottom Line
Warfarin and antibiotics don’t mix safely unless you’re watching your INR closely. No antibiotic is truly "safe" without a check. Don’t rely on memory. Don’t assume your doctor knows. Ask. Test. Log. Communicate.
It’s not about avoiding antibiotics. It’s about knowing how to use them safely with warfarin. One simple INR test before and after can prevent a life-changing bleed. That’s the difference between managing your health - and being at its mercy.
Can I take amoxicillin with warfarin?
Amoxicillin is generally low-risk for warfarin interactions and usually doesn’t raise INR. But exceptions exist. Always get your INR checked 3 to 5 days after starting amoxicillin, especially if you’re over 75, have cancer, or your baseline INR is already above 2.5.
How long after stopping an antibiotic should I check my INR?
Check your INR 7 to 10 days after stopping any antibiotic, even if you feel fine. When the antibiotic is gone, your gut bacteria start making vitamin K again. This can cause your INR to drop suddenly - sometimes into the danger zone for clots. Don’t wait for symptoms.
Is azithromycin safe with warfarin?
Yes, azithromycin is one of the safest macrolide antibiotics to take with warfarin. It doesn’t significantly inhibit liver enzymes or disrupt gut vitamin K. Studies show it affects INR in less than 2% of users. Still, if you’re high-risk, a single INR check 5 days after starting is a good idea.
What should I do if my INR spikes above 5.0?
If your INR is above 5.0, contact your doctor immediately. Do not stop warfarin on your own. You may need vitamin K (oral or IV) to reverse the effect. If you’re bleeding - nosebleeds, bruising, dark stools, headaches - go to the ER. INR above 5.0 is a medical emergency.
Can I use herbal supplements while on warfarin and antibiotics?
Avoid them. Supplements like garlic, ginkgo, ginseng, and vitamin K pills can interfere with warfarin - and that risk multiplies when antibiotics are involved. Even "natural" doesn’t mean safe. Always tell your doctor what you’re taking.
Why do some doctors still prescribe high-risk antibiotics without checking INR?
Many aren’t aware of the specific risks. A 2020 study found only 48% of primary care providers correctly identified high-risk antibiotics. Others assume the patient’s INR is stable or that the antibiotic is "safe." But warfarin interactions are unpredictable. Waiting for symptoms to appear is dangerous. Proactive INR checks save lives.

Wow so antibiotics are just evil now? Next they’ll say water causes bleeding