Bisphosphonate Calcium Timing Calculator
How to Use This Tool
Enter the time you take your bisphosphonate. This calculator shows the minimum time you must wait before taking calcium to avoid absorption problems.
Enter your bisphosphonate time to see safe calcium window
Real-World Examples
Why Your Bisphosphonate Might Not Be Working
You’re taking your bisphosphonate every morning like your doctor said. You’re also taking your calcium supplement because you know it’s good for your bones. So why aren’t your bone density scans improving? The problem isn’t that the medication doesn’t work-it’s that you’re probably taking it at the wrong time.
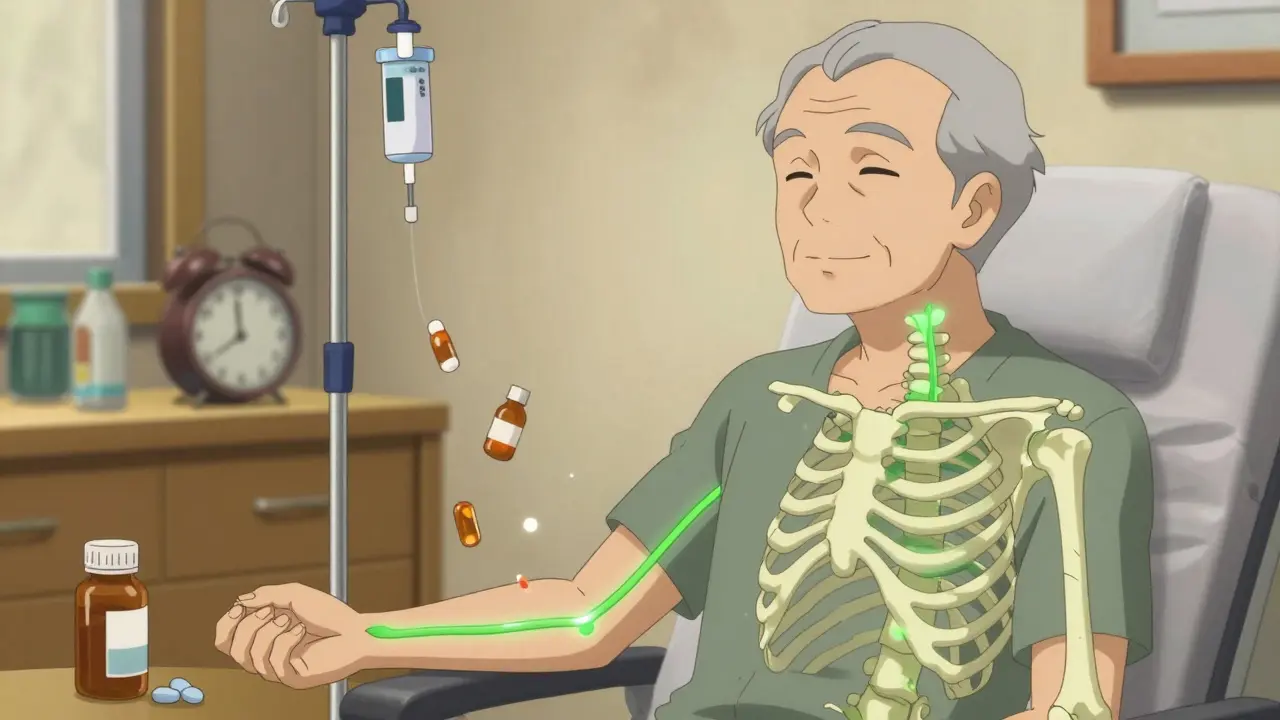
Bisphosphonates like alendronate, risedronate, and zoledronic acid are powerful drugs designed to slow bone loss in osteoporosis. But they’re also incredibly picky. These drugs absorb so poorly in your gut that less than 1% of the dose actually enters your bloodstream-unless you follow the rules exactly. And one of the biggest rule-breakers? Taking calcium at the same time.
The Science Behind the Conflict
Bisphosphonates are built to stick to calcium. That’s not a bug-it’s the whole point. These drugs latch onto areas in your bones where old bone is being broken down, helping to stop the process. But that same chemical design means they’ll also bind to calcium in your stomach or intestines if it’s around.
When you swallow a calcium supplement, tablet, or even a glass of milk right before or after your bisphosphonate, the two form an insoluble complex. It’s like mixing oil and water-your body can’t absorb either properly. Studies show this single mistake can cut bisphosphonate absorption by 90% to 100%. That means you’re taking a $35 pill and getting almost no benefit.
It doesn’t matter if it’s calcium carbonate or calcium citrate. Both interfere. Even antacids, iron pills, or multivitamins with zinc or magnesium can block absorption. The phosphate groups in bisphosphonates are like magnets for any divalent cation. And your gut doesn’t distinguish between the calcium in your bone and the calcium in your supplement.
The Exact Rules You Must Follow
If you’re on an oral bisphosphonate, here’s what you need to do-no exceptions:
- Take your medication first thing in the morning, on an empty stomach. That means no food, coffee, juice, or even water for at least 8 hours before.
- Swallow the pill with a full glass (6-8 oz) of plain tap water. Don’t use sparkling water, mineral water, or any other liquid.
- Stay upright-sitting or standing-for at least 30 to 60 minutes after taking it. Lying down increases the risk of the pill irritating your esophagus.
- Wait at least 30 minutes (preferably 60) before eating, drinking anything else, or taking any other medication, including calcium.
- Only after that window can you take your calcium supplement.
This isn’t a suggestion. It’s based on pharmacokinetic studies from the FDA and the Journal of Clinical Endocrinology & Metabolism. Skip even one step, and you risk rendering the drug useless.
What About the Once-Yearly Shot?
If the daily routine feels impossible, you’re not alone. About half of patients don’t take their oral bisphosphonates correctly, according to the National Osteoporosis Foundation. That’s why many doctors now recommend the yearly intravenous infusion of zoledronic acid (Reclast).
Since it goes straight into your vein, there’s no stomach to interfere with. No fasting. No waiting. No calcium timing headaches. The drug reaches your bones directly, with 100% bioavailability. Studies show adherence jumps from 52% for daily pills to 78% with the yearly shot.
It’s not perfect-it can cause flu-like symptoms for a day or two after the infusion-but for many older adults, especially those juggling multiple medications, it’s a game-changer. And if you’ve already tried oral bisphosphonates and failed to stick to the rules, this might be your best option.

When to Take Calcium (And What Kind)
Calcium isn’t the enemy. You still need it-about 1,200 mg per day if you’re over 50. But timing matters more than the type.
Calcium citrate absorbs better than calcium carbonate when taken with food, and it’s gentler on the stomach. But neither works if you take it too close to your bisphosphonate. The solution? Pick one time each day for calcium-say, lunch or dinner-and make it a habit.
For example: take your bisphosphonate at 5:00 a.m. with water, stay upright for an hour, then go back to bed. Eat breakfast at 7:00 a.m., and take your calcium with your evening meal. That gives you a 12-hour gap. Perfect.
Some people set alarms. Others use pill organizers with labeled compartments. One patient on Reddit posted a 1,400-upvote thread titled “The 30-Minute Rule: How I Finally Got It Right,” where he uses his coffee maker’s timer to remind him when to take his pill.
What If You Messed Up?
Accidentally took your calcium with your bisphosphonate? Don’t panic. Don’t double up. Just wait until tomorrow.
Skipping a dose because you made a mistake is worse than taking it wrong once. The drug has a long half-life in bone tissue-zoledronate can stay active in your skeleton for over 146 hours. One missed absorption window won’t undo weeks of treatment.
But if it happens often, it’s time to reassess. Are you taking it at night? Are you grabbing your multivitamin with breakfast? Are you forgetting because you’re on a dozen other meds? Talk to your pharmacist. They can help you map out a daily schedule that works with your life, not against it.
What About Vitamin D?
You can’t take bisphosphonates without enough vitamin D. If your levels are below 30 ng/mL, your body can’t absorb calcium properly-even if you’re taking it at the right time. That can trigger hypocalcemia, which causes muscle cramps, tingling, and even heart rhythm problems.
Doctors are supposed to check your 25-hydroxyvitamin D level before starting bisphosphonates. If they didn’t, ask for it. Most people need 800-1,000 IU of vitamin D daily. That’s usually included in a good multivitamin, but if you’re over 70 or live in a northern climate, you might need more.
Why This Problem Is Getting Worse
Bisphosphonates are still the most prescribed osteoporosis drugs in the U.S., making up nearly half the market. But patient frustration is rising. Healthgrades ratings show they average just 2.8 out of 5 stars for “ease of use,” mostly because of the timing rules.
Meanwhile, newer drugs like romosozumab (Evenity) don’t have these restrictions. They’re more effective at building bone and have 85% higher adherence rates. But they cost $1,850 a month-over 50 times more than generic alendronate.
So while the future may lie in easier-to-take alternatives, right now, bisphosphonates are still the most affordable and proven option. That means getting the timing right isn’t optional-it’s the difference between preventing a fracture and ending up in the hospital.
What Works in Real Life
Here’s what the data says about real-world success:
- Patients who get a 12-15 minute counseling session with their doctor at the start of treatment are 40% more likely to follow the rules.
- Those who work with a pharmacist for medication therapy management see a 37% drop in errors.
- People who tie their calcium intake to a fixed daily event-like dinner-reduce mistakes by 68%.
- Once-yearly infusions boost adherence from 38% to 72%.
The key isn’t willpower. It’s systems. Write it down. Set a phone alarm. Use a pill box. Tell a family member. Make it automatic.
Final Thought: This Is a Habit Problem, Not a Medication Problem
Bisphosphonates aren’t broken. The system around them is.
Doctors assume patients will read the label. Pharmacists assume the doctor explained it. Patients assume it’s just like any other pill. But this isn’t like taking a statin or a blood pressure pill. This is like threading a needle while running.
If you’re struggling, you’re not failing. You’re just stuck in a system that wasn’t designed for real life. The good news? There are solutions. Talk to your doctor about switching to the yearly shot. Ask your pharmacist to help you map out a schedule. Use reminders. And if you’ve been taking calcium with your bisphosphonate for months? Stop today. Wait 30 minutes next time. Your bones will thank you.


I used to take my alendronate with my morning coffee like a champ... until my bone scan showed zero improvement. Turns out, coffee + calcium = total waste. Now I take it at 5 a.m. with water, wait an hour, then eat. No more guessing. My DEXA scan last year? Up 4%. Small wins, folks.