Every year, tens of thousands of people end up in emergency rooms because they took a supplement with their medicine-without knowing it could be dangerous. It’s not just about herbal teas or vitamin pills. It’s about real, life-threatening risks hiding in plain sight. You might think, It’s natural, so it’s safe. But that’s exactly the myth that puts people in danger.
Why This Isn’t Just a ‘Maybe’ Risk
More than three in four adults in the U.S. take at least one dietary supplement while also on prescription medication. That’s not a small group. That’s millions of people mixing things that haven’t been tested together. Unlike drugs, supplements don’t need FDA approval before they hit the shelf. No safety checks. No interaction studies. Just a label, a price tag, and a promise.
St. John’s wort is the most dangerous offender. It doesn’t just interfere with one or two drugs-it messes with dozens. It can slash the effectiveness of birth control by 40-50%, drop HIV drug levels by over half, and make transplant meds useless. One study showed organ transplant patients taking St. John’s wort had a 50-60% drop in cyclosporine levels. That’s not a typo. That’s rejection risk. And it’s not rare. People report this on forums, in doctor’s offices, and in emergency rooms.
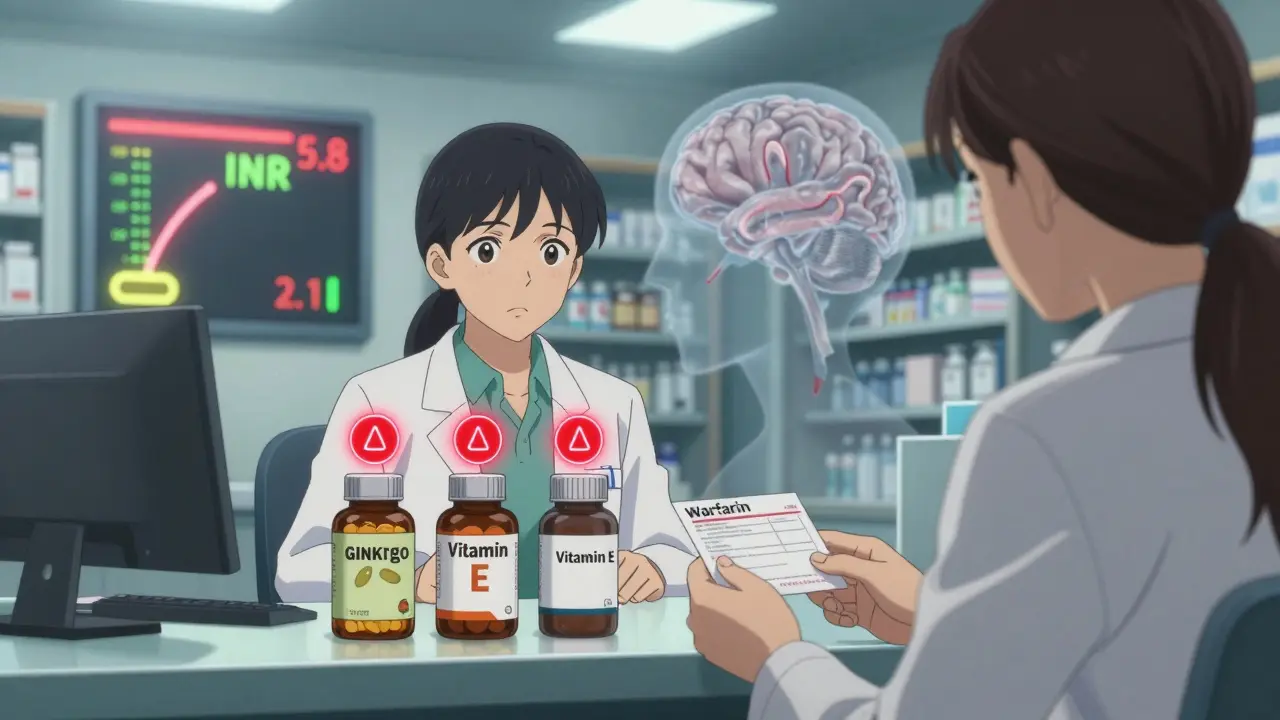
Even something as simple as vitamin E can be risky. At doses above 400 IU per day, it thickens the blood-thinning effect of warfarin. That means more bruising, more nosebleeds, even internal bleeding. Ginkgo biloba? It does the same thing. In one study, 73% of people on warfarin who took ginkgo needed their dose changed. That’s not a coincidence. That’s a red flag.
What You Need to Ask Before Taking Anything
Don’t assume your doctor knows what you’re taking. Studies show most doctors spend less than 90 seconds discussing supplements during a typical visit. You have to be the one to speak up. Here are the seven questions you need to ask yourself-or better yet, write them down and bring them to your pharmacist or doctor.
- Does this supplement affect how your body processes drugs? Many supplements alter enzymes in your liver-especially CYP3A4. St. John’s wort turns this enzyme on full blast, making your body flush out meds like birth control, antidepressants, or HIV drugs too fast. If your drug’s label says “metabolized by CYP3A4,” assume any supplement that affects this enzyme is risky.
- Could this make the effect of my medicine too strong? Ginkgo, garlic, ginger, and high-dose vitamin E all thin the blood. If you’re on warfarin, aspirin, or clopidogrel, adding these increases bleeding risk. Your INR (a blood test that measures clotting time) could spike without warning. One case report showed INR levels jumping from 2.5 to 3.5 just from ginkgo + warfarin.
- Has this supplement been studied with my exact medication? Only about 15% of supplements have any real research on interactions with prescription drugs. If you’re on immunosuppressants, cancer drugs, or anticonvulsants, the chances are even lower. Don’t guess. Check. Use trusted sources like the NIH’s Office of Dietary Supplements or LiverTox.
- Is there a safer alternative? Not all ginseng is the same. Asian ginseng can raise blood pressure and interfere with blood thinners. American ginseng doesn’t. Not all fish oil is equal-some brands are high in vitamin A, which can be toxic with certain meds. Ask your pharmacist: “Is there a version of this supplement that’s less likely to interact?”
- What should I monitor? If you’re on warfarin, get your INR checked regularly. If you’re on HIV meds, watch for viral load spikes. If you’re on antidepressants, know the signs of serotonin syndrome: confusion, fast heartbeat, muscle stiffness, fever. These aren’t side effects-they’re emergencies.
- What symptoms mean something’s wrong? Serotonin syndrome from mixing St. John’s wort with SSRIs like Prozac or Zoloft isn’t rare. Reddit alone has over 140 documented cases since 2022. Don’t wait for a hospital visit. If you feel off after starting a supplement, stop it and call your doctor.
- Have I told my pharmacist? Pharmacists are the unsung heroes of drug safety. They see every prescription you fill. They run interaction checks you never even knew existed. Yet only 32% of doctors document supplement use in medical records. Your pharmacist doesn’t need an invitation. Bring your bottle. Show them the label. Ask: “Is this safe with my meds?”
Who’s Most at Risk?
It’s not just older people. It’s anyone on critical meds:
- Transplant patients on cyclosporine or tacrolimus: One supplement can trigger rejection.
- Cancer patients on chemo: Some supplements may reduce drug effectiveness or increase toxicity.
- People on blood thinners: Even “mild” herbs like garlic or ginger can push INR into dangerous territory.
- Women on birth control: St. John’s wort has caused unplanned pregnancies. Not because of failure-but because the pill stopped working.
- People with HIV: A 57% drop in indinavir levels means the virus can rebound. That’s not theoretical-it’s documented.
These aren’t edge cases. These are real, preventable disasters.
What’s Being Done-and What’s Not
The FDA can’t force supplement makers to prove safety before selling. The industry spends over $50 billion a year, yet less than 3% of products have any documented interaction profile. Labels often lie. A 2022 government report found 70% of supplement labels misstate ingredient amounts. That means you could be taking twice the dose you think.
Some progress is happening. Epic’s electronic health records now require doctors to document supplement use. The CDC is pushing to cut supplement-related ER visits by 25% by 2026. Pharmacists are screening for interactions more often-but most patients never even know it’s happening.
Meanwhile, the debate rages. The Council for Responsible Nutrition claims severe interactions are “exceedingly rare.” But when 23,000 people end up in the ER each year because of supplements, “rare” doesn’t feel right. And when a woman gets pregnant because her birth control stopped working after taking St. John’s wort, “rare” feels like negligence.
What You Can Do Today
You don’t need to stop supplements. You just need to stop guessing.
- Make a list: Every pill, capsule, powder, or tea you take-even if it’s “just for sleep” or “a little magnesium.”
- Bring it to your next appointment: Don’t wait for your doctor to ask. Show them.
- Ask your pharmacist: They’re trained for this. They’re not judging. They’re protecting you.
- Check reliable sources: NIH’s Office of Dietary Supplements, LiverTox, or the American Society of Health-System Pharmacists. Avoid blog posts and Instagram influencers.
- Stop St. John’s wort if you’re on any prescription drug. Seriously. Just stop. It’s not worth the risk.
Supplements aren’t evil. But they’re not harmless either. They’re powerful. And like any powerful thing, they need respect.

Real Stories, Real Consequences
One woman on Reddit wrote: “I didn’t realize St. John’s wort would make my birth control fail. I got pregnant because of it. Doctors never mentioned this risk.”
Another, on Drugs.com: “I took ginkgo for memory after my stroke. My INR went from 2.1 to 5.8. I ended up in the ER with a brain bleed.”
These aren’t outliers. They’re symptoms of a broken system. You’re not alone in not knowing. But you can be the one who changes it-by asking the right questions.
Can I take vitamin D with my blood pressure medicine?
Yes, vitamin D generally doesn’t interfere with most blood pressure medications. But if you’re on calcium-channel blockers like verapamil or diltiazem, high doses of vitamin D can raise calcium levels too much, which might affect heart rhythm. Stick to the recommended dose (600-800 IU/day) and get your blood calcium checked if you’re taking more than 2,000 IU daily.
Is magnesium safe with heart medications?
It depends. Magnesium can lower blood pressure and slow heart rate. If you’re on beta-blockers (like metoprolol) or digoxin, extra magnesium can make those effects stronger. That could lead to dizziness, low pulse, or even heart rhythm problems. Always check with your doctor before taking more than 350 mg of magnesium daily from supplements.
Does fish oil interact with blood thinners?
Yes. Fish oil has mild blood-thinning properties. When combined with warfarin, aspirin, or clopidogrel, it can increase bleeding risk. It’s not always dangerous-but it’s unpredictable. If you’re on a blood thinner, talk to your doctor before starting fish oil. They may check your INR more often or adjust your dose.
Can I take melatonin with antidepressants?
Melatonin is generally low-risk with most antidepressants. But if you’re taking SSRIs like fluoxetine or sertraline, there’s a small chance it could increase serotonin levels too much-leading to serotonin syndrome. Symptoms include agitation, sweating, rapid heartbeat, and confusion. Start with the lowest dose (0.5-1 mg) and watch for side effects. Avoid if you’ve had serotonin syndrome before.
Why don’t doctors warn me about supplements?
Most doctors don’t ask because they assume patients won’t tell them. A 2022 study found doctors spend just 1.2 minutes discussing supplements during a 15-minute visit. They’re not ignoring you-they’re overwhelmed. That’s why you need to bring it up. Write down what you take. Show them the bottles. Make it easy for them to help you.
Are “natural” supplements safer than prescription drugs?
No. “Natural” doesn’t mean safe. St. John’s wort, kava, and comfrey are all natural-and all have caused serious liver damage, seizures, or drug interactions. Prescription drugs go through years of testing. Supplements? One company can make a product, slap a label on it, and sell it without proving it’s safe or effective. That’s the law.
What if I’ve already been taking a supplement with my meds?
Don’t panic. Stop the supplement and call your doctor or pharmacist. Don’t wait for symptoms. Even if you feel fine, the interaction could be building slowly. If you’re on warfarin, HIV meds, or transplant drugs, get tested. Blood tests can show if your drug levels have dropped or if your body is reacting. Better safe than sorry.
Next Steps: Protect Yourself
Start today. Grab your supplement bottles. Write down every name, dose, and reason you take them. Bring them to your next appointment-even if it’s just a checkup. Ask your pharmacist to run a free interaction check. That’s what they’re there for.
Don’t let the myth of “natural equals safe” put your health at risk. You don’t need to quit supplements. You just need to know what you’re mixing. And that knowledge? It could save your life.


I’ve been on warfarin for five years, and I never even thought to mention my fish oil to my pharmacist. Then one day, my INR spiked to 5.2. Turned out the brand I was using had triple the omega-3s listed on the label. I now keep all my supplements in a ziplock with a sticky note that says: “ASK THE PHARMACIST.” No more guessing.