Did you know that up to 30% of all dementia diagnoses are linked to problems with the brain’s blood vessels? That makes vascular dementia a major public‑health challenge, yet many clinicians still reach for drugs originally designed for Alzheimer’s disease. One of those drugs, Donepezil, has been studied for its potential to slow cognitive loss in this vascular form.
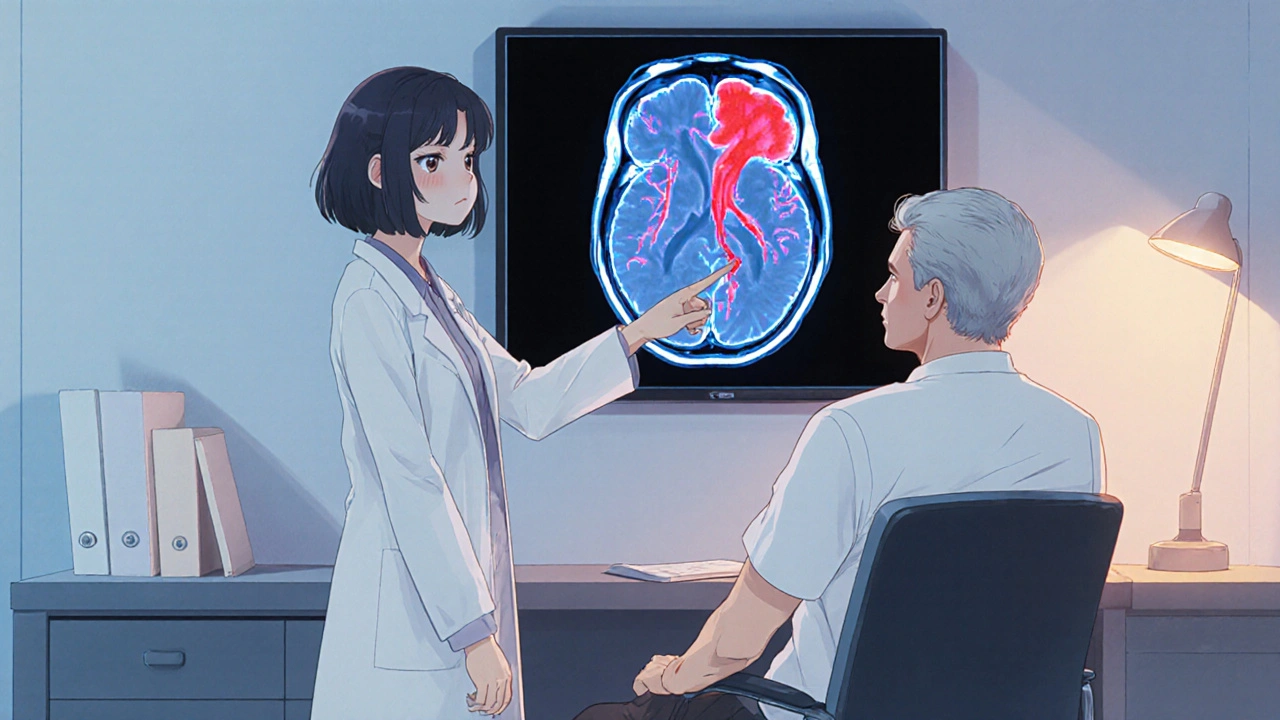
What is Vascular Dementia?
Vascular Dementia is a type of cognitive impairment caused by reduced blood flow to the brain, often after a stroke or a series of small vessel injuries. The condition typically presents with stepwise decline, executive dysfunction, and problems with attention. Unlike Alzheimer’s disease, the pathology is rooted in vascular lesions that can be seen on MRI scans.
Donepezil - A Quick Overview
Donepezil is an acetylcholinesterase inhibitor (AChEI) approved by the FDA in 1996 for mild‑to‑moderate Alzheimer’s disease. By blocking the enzyme that breaks down acetylcholine, it boosts cholinergic signaling, which is essential for learning and memory.
How Donepezil Works in the Brain
The cholinergic hypothesis suggests that many forms of dementia share a deficit in acetylcholine. Donepezil binds reversibly to acetylcholinesterase, raising acetylcholine levels in synaptic clefts. This enhanced signaling can improve attention, processing speed, and short‑term memory-functions that are often compromised in vascular dementia as well.

Clinical Evidence for Donepezil in Vascular Dementia
Several randomized controlled trials have explored Donepezil beyond Alzheimer’s. A 2022 multicenter study involving 312 participants with confirmed vascular dementia showed a modest but statistically significant 2‑point improvement on the Mini‑Mental State Examination (MMSE) after 24 weeks of 10 mg daily dosing compared to placebo. The benefit persisted in a 12‑month extension, though the effect size tapered over time.
Key takeaways from the trial data:
- Improvement in MMSE scores ranged from 1.8 to 2.5 points versus a 0.3‑point decline in the placebo group.
- Patients reported better daily functioning on the Alzheimer’s Disease Cooperative Study‑Activities of Daily Living (ADCS‑ADL) scale.
- Adverse events were mostly mild gastrointestinal issues (nausea, diarrhea) and occurred in 15% of the treatment arm.
Meta‑analyses published in 2023 and 2024, pooling data from six trials, echo these findings, indicating a small but consistent cognitive benefit. Importantly, the studies also highlight that Donepezil does not worsen vascular risk factors such as blood pressure or cholesterol.
Dosing, Administration, and Monitoring
Standard dosing mirrors the Alzheimer’s regimen: start with 5 mg once daily for four weeks, then increase to 10 mg if tolerated. In renal or hepatic impairment, a lower maintenance dose (5 mg) may be prudent.
Clinicians should monitor:
- Baseline MMSE or Montreal Cognitive Assessment (MoCA) to gauge initial severity.
- Weight and gastrointestinal symptoms at each follow‑up (usually 6‑week intervals).
- Potential drug interactions, especially with anticholinergic medications.
Blood tests are not required for routine Donepezil use, but liver function tests are advisable if the patient has pre‑existing hepatic disease.
Benefits vs. Risks - A Balanced View
Benefits:
- Modest improvement in global cognition (MMSE +2 points).
- Better daily functioning, which can delay institutionalization.
- Favorable safety profile compared with other AChEIs for older adults.
Risks:
- Gastrointestinal upset - nausea, vomiting, diarrhoea.
- Rare cardiac effects (bradycardia, syncope) in patients with conduction abnormalities.
- Potential for insomnia or vivid dreams, especially at higher doses.
The decision to start Donepezil should weigh these factors against the patient’s overall health, comorbidities, and goals of care.
How Donepezil Stacks Up Against Other AChE Inhibitors
| Drug | Typical Dose | Evidence Strength (Vascular Dementia) | Common Side Effects | Best For |
|---|---|---|---|---|
| Donepezil | 5‑10 mg daily | Moderate - multiple RCTs, meta‑analysis | Nausea, insomnia, bradycardia | Patients needing once‑daily dosing |
| Rivastigmine | 1.5‑6 mg twice daily or patch | Low - few small trials | Gastro‑intestinal, skin irritation (patch) | Patients who prefer patch administration |
| Galantamine | 16‑24 mg daily | Low - limited vascular data | Vomiting, weight loss | Patients also benefitting from nicotinic modulation |
Overall, Donepezil offers the strongest evidence base for vascular dementia, especially when daily adherence is a concern.
Practical Guidance for Clinicians
1. Confirm Diagnosis: Use MRI or CT to document cerebrovascular lesions and rule out mixed pathology.
2. Baseline Assessment: Record MMSE or MoCA, ADL scores, and cardiovascular status.
3. Start Low, Go Slow: Begin with 5 mg daily, watch for GI upset, then titrate.
4. Re‑evaluate at 12 Weeks: Check cognitive scores and side‑effect profile. If no benefit and tolerability is poor, consider discontinuation.
5. Educate Caregivers: Explain that improvements are modest and that the goal is to maintain function longer rather than cure.
Future Directions
Research is moving toward combination therapy-pairing Donepezil with vascular‑protective agents like cilostazol or antihypertensives to target both the cholinergic deficit and the underlying blood‑flow issue. Ongoing phase‑III trials (expected results 2026) aim to clarify whether such combos can produce synergistic cognitive benefits.
Can Donepezil be used for severe vascular dementia?
Evidence is strongest for mild‑to‑moderate disease. In severe cases, the cognitive gain is minimal and side‑effects may outweigh benefits. Clinicians often pause AChEI therapy at this stage.
How long should a patient stay on Donepezil?
If the patient experiences a stable or improved MMSE score and tolerates the drug, continuation is reasonable. Review effectiveness annually; discontinuation is considered if decline exceeds 3 points per year without other explanations.
Is Donepezil safe for patients on blood thinners?
Yes, there is no direct pharmacologic interaction. However, monitor for any GI bleeding, especially in the elderly, as nausea and vomiting can increase ulcer risk.
What are the most common side effects?
Nausea, diarrhea, insomnia, and occasional bradycardia. Most side effects appear within the first month and often improve with dose adjustment.
Should Donepezil be combined with other dementia drugs?
Combining with memantine is common in Alzheimer’s, but data for vascular dementia are limited. Current guidelines recommend monotherapy unless the patient has mixed pathology.

Donepezil is often presented as a miracle cure for vascular dementia but the reality is more nuanced. The drug works by increasing acetylcholine levels which can help with attention and short term memory. Clinical trials show a modest improvement in MMSE scores around two points after several weeks. That improvement is statistically significant yet clinically modest. The side effect profile is relatively mild with nausea and occasional diarrhea. Some patients report insomnia or vivid dreams especially at higher doses. It does not address the underlying vascular pathology that caused the cognitive decline. Therefore it should be viewed as a symptomatic aid rather than a disease modifying agent. The dosing regimen typically starts low and ramps up to ten milligrams daily if tolerated. Renal and hepatic impairment may require dose adjustments. Monitoring should focus on weight, gastrointestinal symptoms and any cardiac conduction issues. The drug does not appear to worsen blood pressure or cholesterol levels. It is also compatible with most anticoagulants though vigilance for GI bleeding is prudent. Long term studies suggest the benefit may plateau after a year of treatment. In patients with severe vascular dementia the gains are minimal and the risk may outweigh benefit. Ultimately the decision rests on individual tolerance and caregiver goals for maintaining function. The evidence supports a cautious, case‑by‑case use of Donepezil in vascular dementia.