Trying to get pregnant? If you’ve been trying for months without success, don’t overlook your thyroid. It’s not just about ovulation or sperm count - your thyroid hormone levels, especially TSH, play a huge role in whether you can conceive and stay pregnant. Many women are surprised to learn that a TSH level that’s "normal" on a standard lab report might still be too high for optimal fertility.
Why TSH Matters Before Pregnancy
TSH, or thyroid-stimulating hormone, is made by your pituitary gland to tell your thyroid how much hormone to produce. When TSH is too high, your thyroid isn’t making enough T4 and T3 - the hormones that control metabolism, energy, and yes, reproduction. Even mild thyroid underactivity can mess with ovulation, disrupt your menstrual cycle, and make it harder for an embryo to implant.
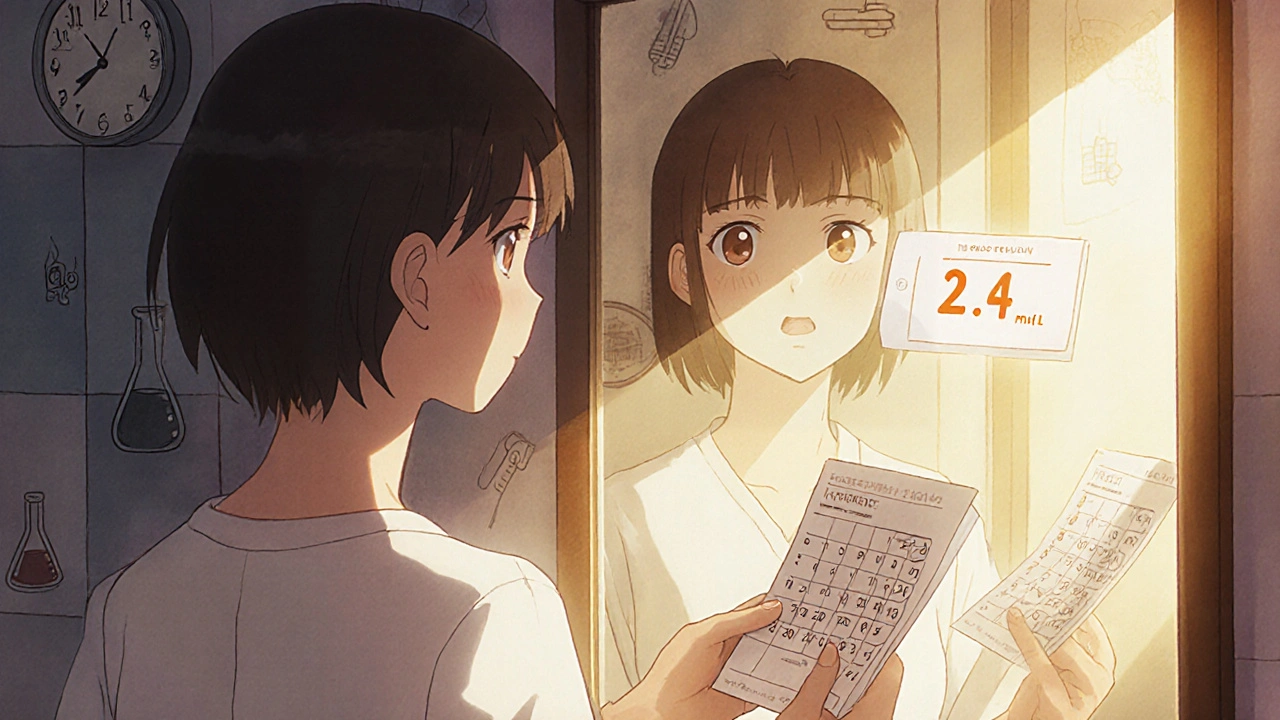
Studies show that women with unexplained infertility are nearly twice as likely to have TSH levels above 2.5 mIU/L compared to women who conceive easily. In one large analysis of over 7,000 women, those with TSH levels between 2.5 and 4.5 mIU/L had a 15% higher chance of miscarriage than those below 2.5. That’s not a small risk - it’s the difference between waiting a few months and losing multiple pregnancies.
The 2.5 mIU/L Target: Where It Comes From
The American Thyroid Association (ATA) set the preconception TSH target at 2.5 mIU/L in 2017 after reviewing dozens of studies. This isn’t the same as the general population range (which can go up to 4.0-4.5 mIU/L). Why the difference? During early pregnancy, your body needs more thyroid hormone to support the baby’s brain development. Your thyroid can’t keep up if it’s already running low.
Women with Hashimoto’s thyroiditis - the most common cause of hypothyroidism - need even tighter control. Research from the ATA’s 2023 patient guidelines suggests aiming for TSH between 1.25 and 1.75 mIU/L before conception. Why? Because your thyroid has to work harder during pregnancy, and if you start with a level close to 2.5, you’ll likely slip into hypothyroidism within weeks of conceiving.
Who Should Get Tested?
The American Society for Reproductive Medicine (ASRM) recommends TSH screening for all women seeking fertility help. But even if you’re not actively trying yet, you should consider testing if you have:
- Family history of thyroid disease
- History of miscarriage (especially two or more)
- Irregular periods or very heavy bleeding
- Unexplained fatigue, weight gain, or cold intolerance
- Autoimmune conditions like type 1 diabetes or celiac disease
Thyroid autoimmunity - meaning you have antibodies attacking your thyroid - affects 10-15% of women with infertility, compared to just 5-8% in the general population. Even if your TSH is normal, those antibodies can raise your miscarriage risk. In fact, pooled data from clinical trials shows that treating these women with levothyroxine reduces miscarriage rates by 45% and boosts live birth rates by 36%.
Levothyroxine: The Only Safe Treatment
If your TSH is too high, your doctor will likely prescribe levothyroxine. This is synthetic T4 - identical to what your thyroid makes. It’s safe, effective, and the only thyroid medication recommended before and during pregnancy.
Don’t use desiccated thyroid (like Armour Thyroid) if you’re trying to conceive. It contains both T4 and T3, but the T3 dose is unpredictable and can cause your serum T4 to drop - which is exactly what you don’t want when your baby’s brain is developing. InVia Fertility Center and the Endocrine Society both warn against it.
Starting dose depends on your weight, age, and current TSH. Most women need a 25-50 mcg increase once they conceive. But here’s the catch: most doctors don’t adjust the dose in time. A 2019 study found only 37% of women on levothyroxine got their dose increased after pregnancy. That means nearly two-thirds are running low when their baby needs it most.
How to Monitor and Adjust
Once you start treatment, don’t just wait until your next annual checkup. TSH levels take about six weeks to stabilize after a dose change. So:
- Get your TSH tested every 4 weeks during preconception optimization
- Once pregnant, test again at 4-6 weeks, then every 6-8 weeks until the second trimester
- Keep your TSH under 2.5 mIU/L before conception, and under 2.5 throughout the first trimester
Some newer guidelines, like those from the European Thyroid Association, suggest even lower targets in early pregnancy: under 1.8 mIU/L in weeks 1-4, under 2.2 by week 8. But for now, sticking to under 2.5 before conception gives you the strongest safety net.
What About Normal TSH But Positive Antibodies?
This is where things get tricky. You can have normal TSH but still have Hashimoto’s. In this case, your risk of miscarriage goes up - even if you feel fine. The ASRM says there’s not enough evidence to treat everyone with normal TSH and antibodies. But many reproductive endocrinologists will still recommend low-dose levothyroxine, especially if you’ve had a prior loss.
A 2023 meta-analysis found that women with thyroid antibodies and TSH above 2.0 had a 2.5x higher miscarriage rate than those with TSH under 2.0. If you’re in this group, ask your doctor: "Would you treat me if I’d already had one miscarriage?" If the answer is yes, then it’s worth considering treatment even before conception.
How to Take Levothyroxine Right
Medication only works if you take it correctly. Levothyroxine is absorbed poorly if you eat too soon after taking it. Here’s what works:
- Take it first thing in the morning on an empty stomach
- Wait at least 30 minutes - ideally 60 - before eating or drinking anything but water
- Avoid calcium, iron, and antacids for at least 4 hours after dosing
- Don’t switch brands without checking with your doctor - different formulations can vary slightly in absorption
Many women report feeling better within 2-4 weeks of starting treatment. But don’t wait to feel better to test your levels. You need lab results to guide dosing, not how you feel.
Cost, Savings, and Real Impact
Levothyroxine costs $4-$10 a month. A single miscarriage can cost over $7,200 in medical care, lost wages, and emotional toll. A 2021 economic study found that optimizing TSH before pregnancy saves $1,850-$2,400 per pregnancy by reducing miscarriages and preterm births.
Think about it: for less than the price of a monthly gym membership, you could prevent a devastating loss. The Global Thyroid Health Initiative estimates that universal preconception screening could prevent 65,000-80,000 miscarriages in the U.S. each year.
What’s Changing in 2025?
The ATA is currently reviewing updated guidelines expected in late 2025. Early drafts suggest more personalized targets based on antibody status and TSH trends over time. A major NIH trial (NCT03856002) wrapping up in late 2024 is testing whether custom TSH goals - not just one number for everyone - improve live birth rates.
One thing won’t change: the need to check TSH before you try to conceive. If you’re planning a pregnancy, this is one of the simplest, cheapest, and most effective steps you can take.
What should my TSH level be before trying to get pregnant?
If you have hypothyroidism or are planning pregnancy, aim for a TSH level below 2.5 mIU/L. Women with Hashimoto’s thyroiditis should target 1.25-1.75 mIU/L. This is lower than the general population range and helps protect early fetal development.
Can I get pregnant with a TSH level of 3.5?
Yes, you can - but your risk of miscarriage increases. Studies show women with TSH between 2.5 and 4.5 mIU/L have a higher chance of pregnancy loss, even if they don’t have thyroid antibodies. Getting your TSH below 2.5 before conception gives you the best shot at a healthy pregnancy.
Do I need to take thyroid medication if my TSH is normal?
Only if you have thyroid antibodies and a history of miscarriage. If your TSH is normal and you have no antibodies, treatment isn’t usually recommended. But if you’ve had unexplained pregnancy loss, your doctor may still suggest low-dose levothyroxine - especially if your TSH is above 2.0.
Can I take levothyroxine with my prenatal vitamin?
No. Prenatal vitamins often contain iron and calcium, which block levothyroxine absorption. Take your thyroid pill at least 4 hours before or after your prenatal vitamin. Best practice: take levothyroxine alone in the morning, then take your prenatal with lunch or dinner.
How often should I get my TSH checked when trying to conceive?
Every 4-6 weeks until your TSH is stable under 2.5 mIU/L. Once you’re pregnant, test again at 4-6 weeks, then every 6-8 weeks through the first half of pregnancy. Dose adjustments are common and necessary - don’t assume your pre-pregnancy dose will be enough.
Is it safe to take levothyroxine during pregnancy?
Yes - it’s not just safe, it’s essential. Untreated hypothyroidism during pregnancy increases the risk of preterm birth, low birth weight, and developmental delays in the child. Levothyroxine is the same hormone your body naturally makes and is considered one of the safest medications to take during pregnancy.
Next Steps
If you’re planning a pregnancy and haven’t had your TSH checked in the last year, schedule a blood test now. Ask for both TSH and thyroid peroxidase antibodies (TPOAb). If your TSH is above 2.5, talk to an endocrinologist or reproductive specialist - don’t wait. This isn’t about being "sick." It’s about giving your future baby the best start possible.
Thyroid health before conception isn’t a luxury. It’s a foundation. And it’s one of the few fertility factors you can control with a simple pill, a blood test, and a few minutes each morning.

So I just got my TSH back at 3.1 and I’ve been trying for 8 months. I thought I was fine because my doctor said it was "normal." Now I’m sitting here wondering if I’ve been wasting time. This post just gut-punched me, but in a good way. I’m scheduling an endo appointment tomorrow. No more "it’s probably just stress."