For women with PCOS and obesity, losing weight isn’t just about appearance-it’s about reversing insulin resistance, lowering testosterone, and getting periods back. But traditional treatments like metformin often fall short. Enter GLP-1 receptor agonists: medications originally made for diabetes that are now turning heads for their powerful effects on weight and metabolism in PCOS. If you’ve struggled to lose weight despite diet and exercise, this isn’t just another trend-it’s science with real numbers behind it.
How GLP-1s Actually Work in Your Body
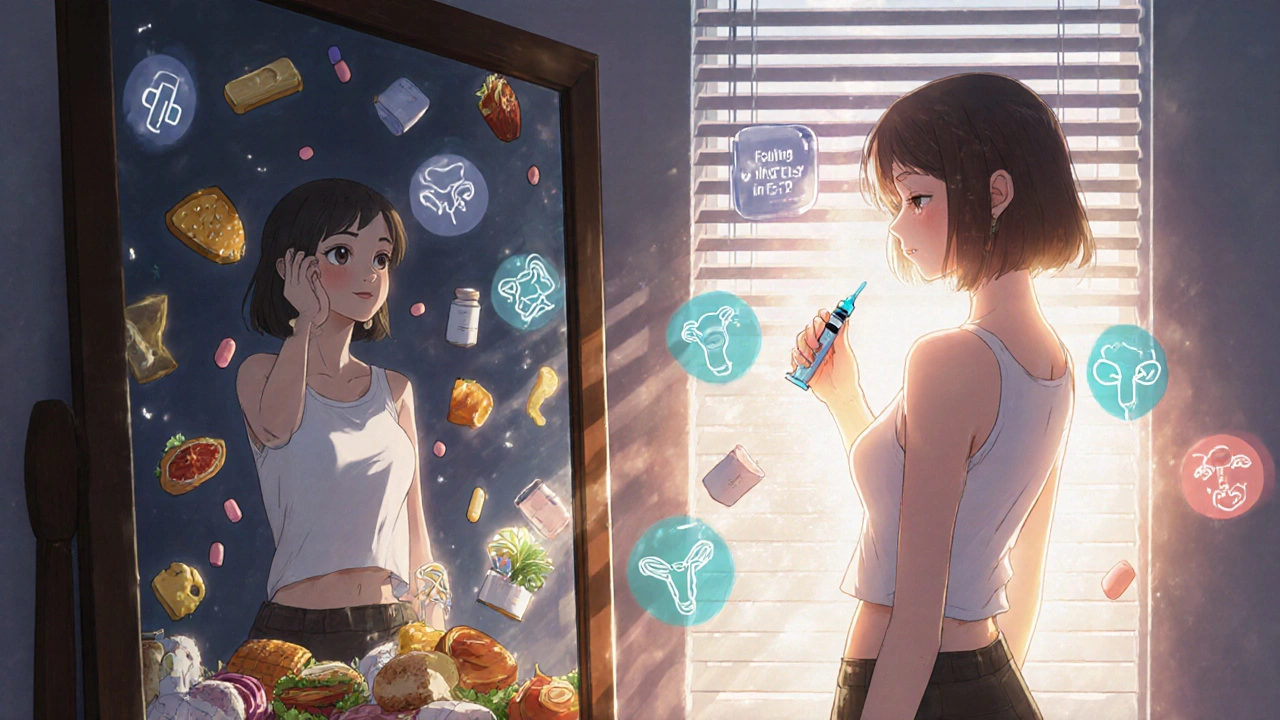
GLP-1s mimic a natural hormone your gut makes after eating. This hormone tells your pancreas to release insulin only when blood sugar is high, slows down how fast food leaves your stomach, and sends a clear signal to your brain: ‘You’re full.’ That’s why you eat less without feeling hungry all the time.
These drugs don’t just affect your gut and pancreas. They cross the blood-brain barrier and act on appetite centers in your hypothalamus. They also reduce fat storage in your liver and around your organs. In women with PCOS, this means less visceral fat-the dangerous kind linked to heart disease and insulin resistance. Studies show GLP-1s can cut visceral fat by up to 18% in just a few months.
Unlike metformin, which mainly improves insulin sensitivity, GLP-1s attack multiple problems at once: appetite, fat storage, blood sugar spikes, and even inflammation. That’s why they’re so effective for PCOS, where these issues stack up.
Weight Loss Numbers You Can Trust
Let’s talk numbers. In clinical trials, women with PCOS using liraglutide (1.8-3.0 mg daily) lost an average of 5-10% of their body weight over 6 months. Those on semaglutide (2.4 mg weekly) lost even more-up to 14.9% over 15 months in the STEP trials. That’s not a few pounds. For someone weighing 200 lbs, that’s 20-30 lbs gone.
Compare that to metformin, which typically leads to 2-4% weight loss. GLP-1s aren’t just better-they’re in a different league. One 2024 study showed semaglutide users lost 10.2% of their weight in 36 weeks, while the placebo group lost just 2.1%. That gap isn’t small. It’s life-changing.
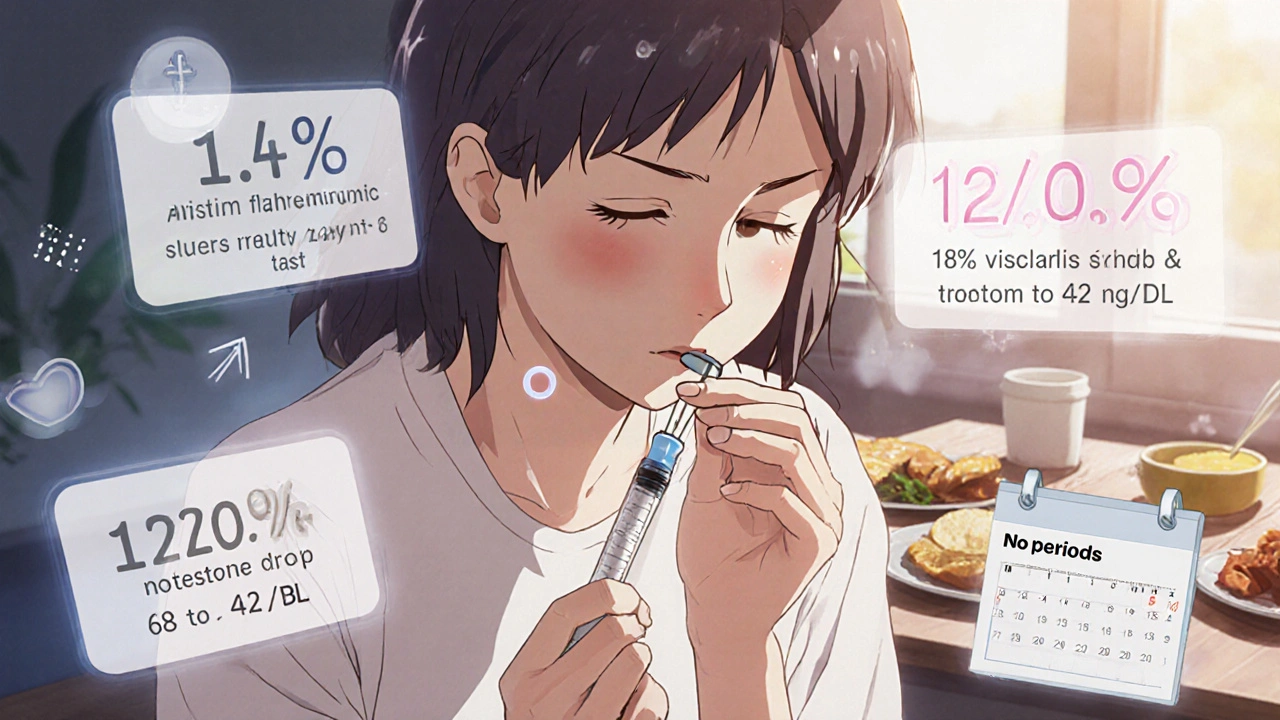
And it’s not just about the scale. Testosterone levels drop. One woman on Reddit reported her testosterone fell from 68 to 42 ng/dL after 6 months on semaglutide. Her period returned after 3 years of absence. These aren’t isolated cases. In a 2022 study, 42% of PCOS patients on liraglutide started ovulating spontaneously. That’s fertility improvement without IVF or clomiphene.
Why GLP-1s Beat Metformin for Weight Loss
Metformin is still the first-line drug for PCOS. It’s cheap, safe, and helps with insulin resistance. But if your goal is significant weight loss, it’s not enough.
Here’s the breakdown:
- Metformin: 2-4% weight loss, modest improvement in insulin sensitivity, little effect on testosterone or visceral fat.
- Liraglutide: 5-10% weight loss, 18% reduction in visceral fat, significant drop in testosterone, improved menstrual regularity.
- Semaglutide: 10-15% weight loss, strong improvement in lipid profile, reduced inflammation markers, higher rates of ovulation.
The difference isn’t just in the numbers-it’s in the quality of life. Women on GLP-1s report less fatigue, fewer cravings, and more energy. Many say they finally feel like they can control their eating for the first time.
And here’s the kicker: even after stopping GLP-1s, women who kept taking metformin regained only one-third of the weight they lost. Those who stopped both medications regained 60-70%. That means combining GLP-1s with metformin isn’t just smart-it’s critical for long-term success.
The Catch: Side Effects and Costs
GLP-1s aren’t magic pills. They come with real downsides.
Nausea is the most common side effect-reported by 44% of users in trials. Vomiting affects 24%, and dizziness hits 15%. Most of these fade after a few weeks as your body adjusts. But for some, they’re enough to quit. On Reddit’s r/PCOS forum, 34% of users said nausea made them stop. One woman wrote: ‘Spent $1,200 a month on Wegovy. Lost 15 lbs but couldn’t keep food down. Switched back to metformin.’
Cost is another barrier. Brand-name semaglutide (Wegovy) and liraglutide (Saxenda) cost $800-$1,400 per month in the U.S. Generic metformin? $10-$20. Even with insurance, copays can be $200-$500. In Australia, these drugs aren’t subsidized for PCOS, so most pay out-of-pocket.
There are also safety limits. You can’t use them if you or a family member had medullary thyroid cancer. They’re not approved for use in pregnancy. And while long-term data for diabetes and obesity is strong, we still don’t have 10-year studies specifically for PCOS.
Who Benefits Most-and Who Doesn’t
GLP-1s work best for women with PCOS who have:
- BMI over 30
- Insulin resistance or prediabetes
- High testosterone or irregular periods
- Failed to lose weight with diet, exercise, or metformin
They’re not as effective for lean PCOS patients-those with normal weight but hormonal imbalances. In those cases, metformin, lifestyle changes, or birth control pills still hold more value.
Also, if you’re planning to get pregnant soon, GLP-1s aren’t the right choice. You need to stop them at least 2 months before trying to conceive. And if you’re on insulin or sulfonylureas, your doctor must adjust those doses to avoid low blood sugar.
How to Start-And How to Stick With It
If your doctor agrees GLP-1s are right for you, here’s how to start:
- Start low. Semaglutide begins at 0.25 mg weekly. Increase by 0.25 mg every 4 weeks until you hit 2.4 mg. Liraglutide starts at 0.6 mg daily, increasing weekly to 1.8-3.0 mg.
- Use the injection correctly. Inject under the skin of your belly, thigh, or upper arm. Rotate sites to avoid irritation.
- Adjust your diet. Eat smaller, protein-rich meals. Avoid greasy or sugary foods-they worsen nausea.
- Stay hydrated. Drink water before and after injections.
- Keep taking metformin. It helps maintain weight loss after you stop the GLP-1.
Most side effects peak in weeks 2-6. If nausea lasts longer than 8 weeks, talk to your doctor. Don’t just quit. They can slow down the ramp-up or suggest anti-nausea meds like ginger or ondansetron.
What’s Coming Next
The future is bright-and fast-moving.
In June 2024, the European Medicines Agency accepted Novo Nordisk’s application to approve semaglutide 2.4 mg specifically for PCOS with metabolic complications. A decision is expected in early 2025. If approved, this would be the first official indication for GLP-1s in PCOS.
Meanwhile, the STEP-PCOS trial (NCT05169358) is tracking 450 women for 72 weeks. Early results show 10.2% weight loss at 36 weeks. That’s better than any drug ever tested for PCOS.
Oral versions of GLP-1s, like Rybelsus, are already available for diabetes and may soon be used off-label for PCOS. That could cut costs and improve adherence. And researchers are testing triple agonists-drugs that hit GLP-1, GIP, and glucagon receptors-that could lead to even bigger weight loss.
By 2027, experts predict GLP-1s will become standard care for obese PCOS patients with metabolic issues. But until then, access remains limited by cost and lack of formal approval.
Final Thoughts: Is It Worth It?
If you’re a woman with PCOS and obesity, and you’ve tried everything else, GLP-1s offer the most powerful metabolic reset you’ve seen. The weight loss is real. The hormone improvements are measurable. The quality-of-life gains are undeniable.
But it’s not for everyone. If you can’t afford it, can’t tolerate nausea, or don’t have insulin resistance, it’s not the answer. Metformin, lifestyle changes, and birth control still have their place.
The key is to treat PCOS as a metabolic disease-not just a reproductive one. GLP-1s don’t cure PCOS. But for many, they’re the first tool that lets you take real control of it.
Can GLP-1s help me get pregnant if I have PCOS?
Yes, in many cases. GLP-1s improve insulin sensitivity and lower testosterone, which helps restore ovulation. Studies show 42% of women on liraglutide started ovulating spontaneously. However, you must stop GLP-1s at least 2 months before trying to conceive. They’re not approved during pregnancy.
How long do I need to take GLP-1s for PCOS?
There’s no fixed timeline. Weight loss happens over 6-12 months, but PCOS is a lifelong condition. Many women stay on GLP-1s long-term, especially if they’re combined with metformin. Stopping often leads to weight regain. Think of it like blood pressure medication-you take it as long as you need to stay healthy.
Are GLP-1s covered by insurance for PCOS?
In most places, no. GLP-1s are only officially approved for type 2 diabetes and obesity-not PCOS. In Australia and the U.S., insurance rarely covers them for PCOS unless you have a BMI over 30 and prediabetes. Even then, prior authorization is hard to get. Most patients pay out-of-pocket.
Can I take GLP-1s with birth control pills?
Yes. There’s no known interaction between GLP-1s and hormonal birth control. Many women take both: birth control to regulate periods and GLP-1s to lose weight and improve insulin resistance. Always tell your doctor you’re on both.
Do GLP-1s cause muscle loss?
Not if you do it right. Some weight loss from any method can include muscle, but GLP-1s are less likely to cause it than extreme dieting. To preserve muscle, eat enough protein (1.6-2.2g per kg of body weight) and lift weights 2-3 times a week. Studies show women on semaglutide who exercised maintained lean mass better than those who didn’t.
What’s the difference between Wegovy and Ozempic?
They’re the same drug-semaglutide-but different doses and approvals. Wegovy is 2.4 mg weekly and approved for obesity. Ozempic is up to 1.0 mg weekly and approved for type 2 diabetes. Some doctors prescribe Ozempic off-label for PCOS at higher doses, but that’s not officially allowed. Stick to the approved dose unless your endocrinologist says otherwise.

OMG I started semaglutide last month and I’m already down 12 lbs!!! 😭💖 My cravings just vanished like magic-no more 3am ice cream binges. My period came back after 4 years. I’m crying typing this. Thank you for this post. 🙏✨