Itchy, raised welts that show up out of nowhere-sometimes after eating peanuts, other times after a hot shower or stress. They burn, they swell, they keep you up at night. If you’ve had hives, you know how unpredictable and frustrating they can be. This condition, called urticaria, affects about 1 in 5 people at some point in their life. For most, it’s a short-lived annoyance. For others, it becomes a daily battle that lasts months or even years.
What Exactly Are Hives?
Hives are not a disease themselves-they’re a reaction. They appear as red, swollen, itchy bumps or patches on the skin, often with a pale center. These welts can be as small as a pinhead or as large as a dinner plate. They move around the body, appearing in one spot, fading, and reappearing elsewhere. The key sign? They usually vanish within 24 hours in the same place, which is why doctors ask, “Do they last longer than a day in the same spot?” If yes, it’s likely not hives. The cause? Mast cells in your skin release histamine. This chemical makes tiny blood vessels leak fluid into the surrounding tissue, causing the swelling and itch. It’s the same reaction your body has when you get stung by a bee-but without the bee.What Triggers Hives?
People often assume hives are always from food allergies. While peanuts, shellfish, or eggs can trigger them, that’s only true for a small number of cases. In fact, less than 20% of chronic hives are caused by identifiable food or environmental allergens. Common triggers include:- Physical stimuli: Heat, cold, pressure, sweat, or even scratching the skin (called dermographism). A hot shower can bring on hives in some people.
- Infections: Viral infections like colds or stomach bugs often precede outbreaks, especially in children.
- Medications: Antibiotics like penicillin, NSAIDs like ibuprofen, and even some blood pressure pills can be culprits.
- Stress: Emotional stress doesn’t cause hives directly, but it can worsen them or make them harder to control.
- Autoimmune activity: In up to 40% of chronic cases, the body’s immune system mistakenly attacks its own mast cells, triggering histamine release without any outside trigger.
Why Antihistamines Are the First Line of Defense
Antihistamines are the go-to treatment for a reason: they block histamine from binding to receptors in your skin. Less histamine activity means less itching, less swelling, fewer hives. There are two main types:- Second-generation antihistamines: Cetirizine (Zyrtec), loratadine (Claritin), fexofenadine (Allegra). These are non-sedating and designed to last 24 hours. Most doctors start here.
- First-generation antihistamines: Diphenhydramine (Benadryl), hydroxyzine. These work fast but cause drowsiness in 50-70% of users. They’re better for nighttime use when sleep is disrupted.

What If Antihistamines Don’t Work?
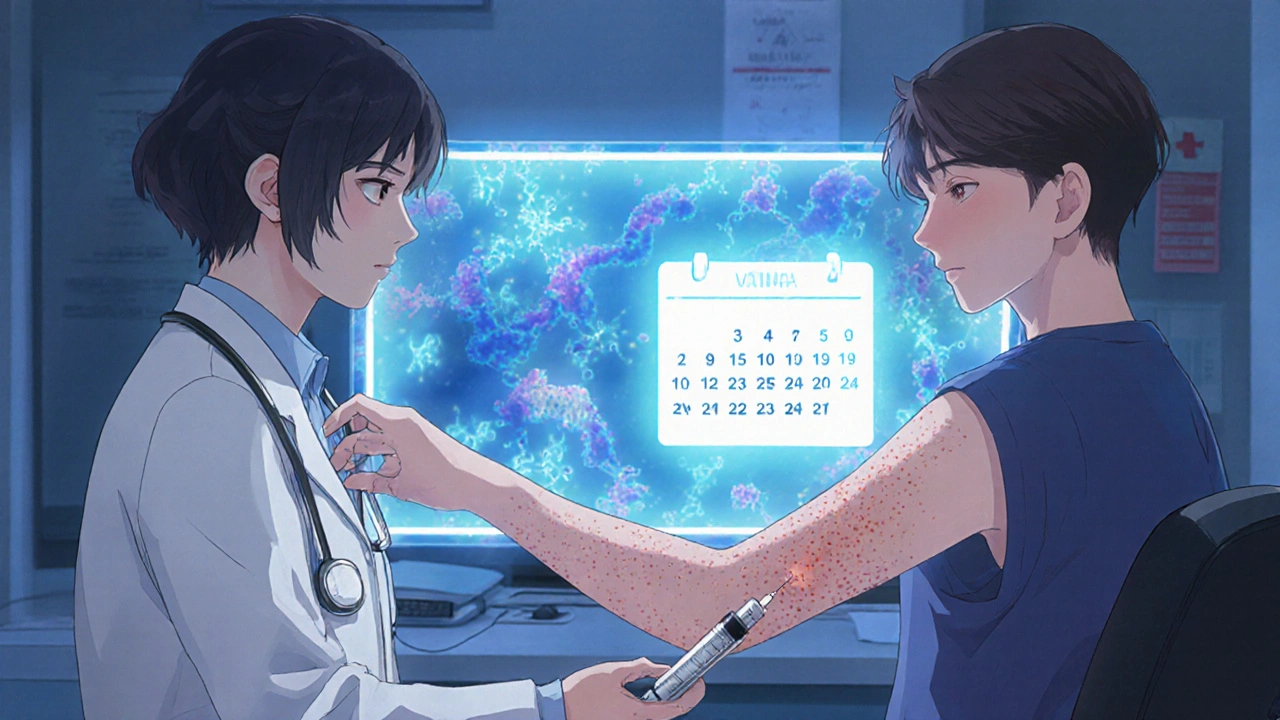
About 30-40% of people with chronic hives don’t respond well to even high-dose antihistamines. That’s when doctors look at other options.- Omalizumab (Xolair): This injectable biologic, approved in 2014, targets IgE antibodies involved in the allergic response. It’s given as a subcutaneous shot every four weeks. Clinical trials show 65% of patients see major improvement, with many achieving complete symptom control within 4-8 weeks. The downside? Cost-around $1,500 per dose in the U.S.-and injection site reactions in about 35% of users.
- Dupilumab (Dupixent): Approved for chronic hives in September 2023, this injectable blocks IL-4 and IL-13, two key inflammation drivers. In trials, 55% of patients had complete resolution of hives, compared to just 15% on placebo.
- Remibrutinib: A new oral medication approved in January 2024, it inhibits a specific enzyme (BTK) involved in mast cell activation. In phase 3 trials, 45% of patients had complete symptom control at 50mg twice daily. Its big advantage? Being a pill instead of an injection improves adherence.
Real Stories, Real Struggles
Online communities like Reddit’s r/ChronicHives (with over 15,000 members) reveal how deeply hives affect daily life. In a 2023 survey of 1,245 members:- 68% said hives disrupted their sleep-many waking up 2-3 times a night.
- 42% avoided social events because they feared visible outbreaks.
- 22% saw three or more doctors before getting the right diagnosis.
How to Get Started Managing Hives
If you’re dealing with hives, here’s a practical plan:- Start with a non-sedating antihistamine: Take cetirizine 10mg once daily for at least 7 days. Don’t stop if you still have some hives-this is normal.
- Track your symptoms: Use a simple notebook or app like ‘Urticaria Tracker’ to log when hives appear, what you ate, stress levels, weather, and activities. Patterns often emerge over 2-4 weeks.
- Don’t self-diagnose triggers: Avoiding gluten or dairy without evidence won’t help if your hives are autoimmune. Focus on identifying physical triggers first-heat, pressure, exercise.
- See an allergist if it lasts more than two weeks: Especially if hives are daily, or if you have swelling of the lips or tongue (angioedema). That’s a red flag.
- Consider combination therapy: If daytime itching is bad but sleep is worse, take a non-drowsy antihistamine in the morning and a low-dose sedating one at night. Studies show this improves control by 30%.
The Bigger Picture
The global market for urticaria treatments is growing fast-projected to hit nearly $3 billion by 2028. That’s because more people are being diagnosed, and new treatments are arriving. But access isn’t equal. In low-income countries, only 30% of chronic hives patients can afford biologics. In high-income places, it’s 85%. New research is pointing toward personalized treatment. Within five years, genetic testing may help doctors choose which antihistamine works best for your body, reducing trial and error. Meanwhile, telemedicine is helping. In 2023, 45% of allergists in the U.S. used virtual visits for hives follow-ups, making care more accessible for people in rural areas.When to Worry
Most hives are harmless. But call a doctor or go to urgent care if you have:- Swelling of the lips, tongue, or throat
- Difficulty breathing or wheezing
- Dizziness or rapid heartbeat
- Hives that last longer than six weeks without improvement
Urticaria isn’t just a skin problem-it’s a disruption to sleep, confidence, work, and relationships. But it’s manageable. With the right approach, most people can regain control. Start with antihistamines, track your triggers, and don’t hesitate to ask for help if things don’t improve. You’re not alone-and better treatments are on the way.
Can stress cause hives?
Stress doesn’t directly cause hives, but it can trigger flare-ups or make existing hives worse. In chronic cases, stress is one of the most common aggravating factors. Managing stress through sleep, exercise, or mindfulness can help reduce outbreak frequency.
Are hives contagious?
No, hives are not contagious. You cannot catch them from someone else. They’re caused by your body’s internal reaction-often to allergens, stress, or autoimmune activity-not by bacteria or viruses.
Can I take antihistamines every day?
Yes, second-generation antihistamines like cetirizine and fexofenadine are safe for daily, long-term use. Many people with chronic hives take them for months or years without side effects. Always follow your doctor’s dosing advice, especially if increasing the dose.
Why do my hives come back at night?
Histamine levels naturally rise at night, and body temperature increases during sleep-both can worsen hives. Also, without distractions, you notice the itching more. Using a sedating antihistamine at night can help break this cycle.
Is there a cure for chronic hives?
There’s no guaranteed cure, but many people go into remission. About 50% of chronic spontaneous urticaria cases resolve within 3-5 years without treatment. Newer medications like remibrutinib and dupilumab are helping more people achieve full control, and research is moving toward identifying root causes, not just managing symptoms.
Should I avoid all processed foods if I have hives?
No, avoiding all processed foods isn’t necessary unless you’ve identified a specific food trigger through testing or elimination. Many people blame food when the real issue is physical triggers like heat or pressure. Focus on tracking patterns first before making major diet changes.


Been dealing with this for 3 years. Took me 11 doctors to finally get diagnosed. The moment I started doubling my cetirizine? Life changed. No more 3am scratching marathons. Also, hot showers are my enemy - now I keep it lukewarm and it’s night and day. Don’t let anyone tell you ‘it’s all in your head.’ It’s biology, not weakness.