It’s been two weeks since you started taking escitalopram, and you’re still feeling the same. Maybe worse. You check your phone for the fifth time today, wondering if it’s working-or if you made a mistake. You’re not alone. Thousands of people start escitalopram each month, hoping for relief from anxiety or depression, only to feel stuck in the waiting game. The truth? It doesn’t work overnight. But it also doesn’t take months. There’s a real timeline, and knowing it can save you from quitting too soon-or staying on longer than you need to.
What escitalopram actually does in your brain
Escitalopram is a selective serotonin reuptake inhibitor, or SSRI. That means it stops your brain from reabsorbing too much serotonin-the chemical linked to mood, sleep, and calm. Think of serotonin like a message runner. Normally, after it delivers its message, it gets picked back up. Escitalopram slows down that pickup, so more messages stay around longer. But your brain doesn’t instantly adapt. It takes time for your neurons to adjust to this new balance. That’s why you don’t feel better right away.
Some people think if a drug doesn’t work in a week, it’s broken. But antidepressants aren’t painkillers. You can’t just wait for the fog to lift. Your brain needs to rebuild its response patterns. That’s why side effects often show up before benefits.
The first two weeks: Side effects before relief
Most people notice side effects within the first few days. Nausea, headaches, dizziness, trouble sleeping, or even increased anxiety. These aren’t signs the drug isn’t working-they’re signs your brain is adjusting. A 2023 meta-analysis in The American Journal of Psychiatry found that over 60% of people starting escitalopram reported mild to moderate side effects in the first 10 days. But only 12% stopped because of them.
These early side effects usually fade by the end of week two. If they get worse or you feel suicidal, talk to your doctor immediately. But if you’re just feeling off, it’s likely part of the process. Don’t quit yet.
Weeks 3 to 6: The slow lift
This is when things start to shift-for most people. Around week three, you might notice small changes: you sleep a little better, you laugh at a joke that used to feel flat, or you get through a workday without feeling drained. These aren’t dramatic. They’re subtle. But they’re real.
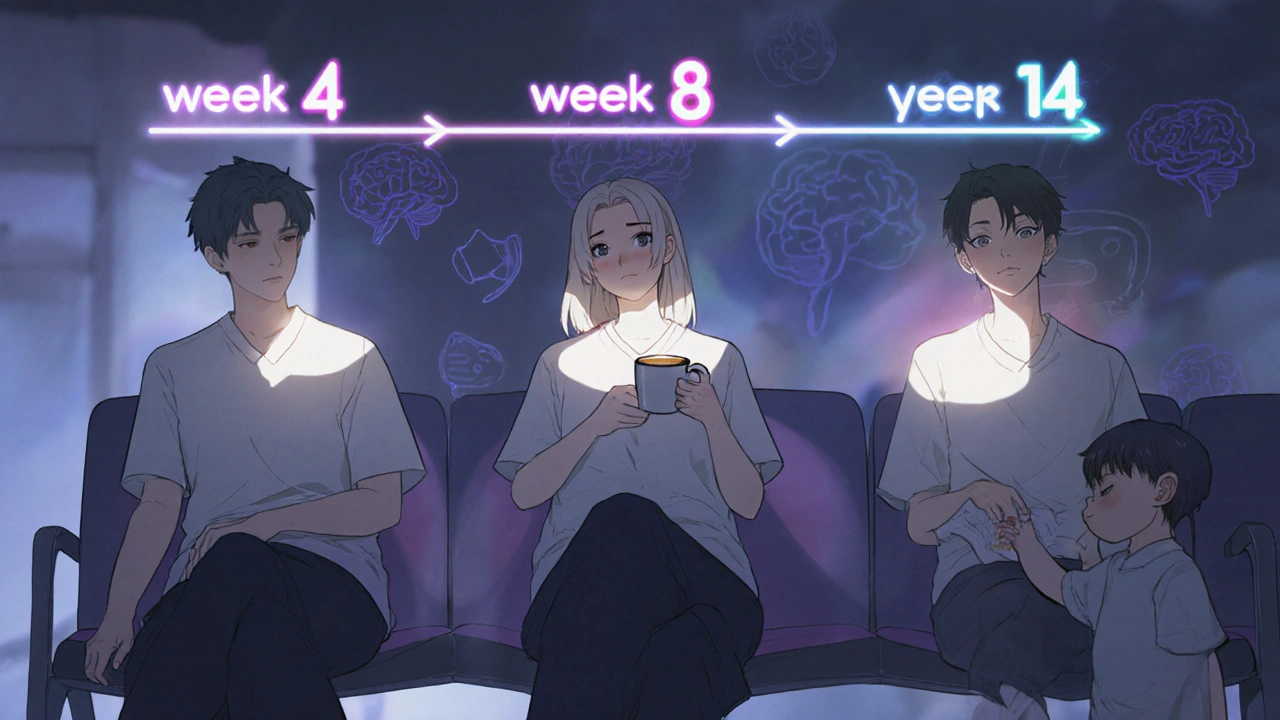
A study following 1,200 patients on escitalopram found that 45% reported noticeable improvement in mood by week four. By week six, that number jumped to 68%. The biggest improvements usually show up in physical symptoms first: less muscle tension, better appetite, more energy. Emotional changes come later.
If you’re still feeling hopeless at week six, that doesn’t mean escitalopram won’t work. It just means you might need more time-or a different dose. Your doctor might adjust your dose between weeks 6 and 8 if there’s no progress. Most people reach their optimal dose by week eight.

Week 8 and beyond: Full effect
By week eight, about 75% of people on escitalopram see a meaningful reduction in symptoms. That’s the point where most doctors consider the medication “fully effective.” If you’re still struggling after 12 weeks, it’s time to revisit your treatment plan. Escitalopram isn’t magic. It works best when paired with therapy, exercise, and good sleep habits.
Some people feel almost completely better by week 10. Others take longer. Age, genetics, how long you’ve had symptoms, and whether you’ve tried other meds before all play a role. There’s no universal clock. But the pattern is consistent: slow, steady, and not linear.
What doesn’t work
Don’t double your dose because you’re impatient. Taking more than prescribed won’t speed things up-it just increases side effects and risks. Don’t switch to another SSRI after two weeks. That’s like changing tires because your car hasn’t reached its destination yet. Don’t compare yourself to someone else’s timeline. One person might feel better at week five; another needs 14 weeks. Both are normal.
Also, don’t assume that feeling better means you can stop. Escitalopram isn’t a quick fix. Stopping suddenly can cause withdrawal symptoms like brain zaps, dizziness, or irritability. Always taper off under medical supervision.
When to call your doctor
There are red flags you shouldn’t ignore:
- Worsening depression or new thoughts of self-harm, especially in the first four weeks
- Severe insomnia or agitation that doesn’t improve after 10 days
- Unexplained muscle stiffness, high fever, or rapid heartbeat (signs of serotonin syndrome)
- No change after 12 weeks, even at the highest tolerated dose
If any of these happen, reach out. Your doctor might switch you to another SSRI like sertraline, or consider adding therapy. Escitalopram isn’t the only option-and it’s not the right one for everyone.
What helps it work faster
While you wait for escitalopram to take effect, you’re not powerless. These habits can help:
- Get 7-8 hours of sleep every night. Poor sleep blocks antidepressants from working properly.
- Move your body daily. Even a 20-minute walk boosts serotonin naturally.
- Reduce caffeine and alcohol. Both interfere with how your brain responds to SSRIs.
- Try cognitive behavioral therapy (CBT). Studies show CBT combined with escitalopram works better than either alone.
There’s no shortcut, but you can make the wait more bearable-and more effective.
Real stories, real timelines
Emma, 34, from Sydney, started escitalopram after months of panic attacks. She felt worse for the first 10 days. By week five, she could leave the house without shaking. At week nine, she went back to work full-time.
Mark, 51, took escitalopram for chronic low mood. He didn’t feel a difference until week 11. He thought it wasn’t working. His doctor told him to stick with it. By week 14, he started noticing he smiled more at his grandkids.
Both got better. Neither got better on the same schedule. That’s the point.
Final thoughts
Escitalopram takes time-not because it’s slow, but because healing your brain isn’t a sprint. It’s a quiet rebuild. Most people start feeling better between weeks 4 and 8. Full results usually arrive by week 12. If you’re still waiting past that, it’s not failure-it’s a signal to talk to your doctor.
Don’t give up too early. Don’t wait too long. And don’t assume you’re broken because it’s not instant. You’re not. You’re just in the middle of a process that takes patience, not magic.
Can escitalopram work in one week?
It’s extremely rare for escitalopram to work in one week. Most people don’t notice any mood improvement until at least week three. Early changes, if they happen, are usually subtle-like better sleep or less physical tension. Don’t expect emotional relief this early. If you feel worse, contact your doctor.
Why do I feel worse before I feel better?
Escitalopram increases serotonin levels quickly, but your brain needs weeks to adapt to that change. In the meantime, some neural pathways become overstimulated, leading to increased anxiety, nausea, or insomnia. This is temporary for most people and usually fades by week two. If it gets worse or you have suicidal thoughts, tell your doctor right away.
Is 10 mg of escitalopram enough?
Ten milligrams is the standard starting dose for most adults. For many, it’s enough. But some people need 15 or 20 mg for full effect. Your doctor will adjust your dose based on your response and side effects. Never increase the dose on your own. If you’ve been on 10 mg for 8 weeks with no improvement, talk to your doctor about a possible increase.
Does escitalopram make you feel numb?
Some people report feeling emotionally flat or detached while on escitalopram. This isn’t the same as feeling better-it’s a side effect called emotional blunting. It’s more common at higher doses and can be managed by lowering the dose or switching medications. If you feel like you’re not yourself, discuss it with your doctor. It’s not permanent, and it’s treatable.
What happens if I stop escitalopram too soon?
Stopping escitalopram abruptly can cause withdrawal symptoms like dizziness, nausea, brain zaps, irritability, or sleep problems. These can last days to weeks. Even if you feel fine, stopping before 6-12 months of stability increases your risk of relapse. Always taper off slowly under medical supervision, even if you think you’re cured.
Can I drink alcohol while taking escitalopram?
It’s not recommended. Alcohol can worsen depression and anxiety symptoms, interfere with sleep, and increase side effects like dizziness and drowsiness. It also reduces the effectiveness of escitalopram. If you drink occasionally, limit it. If you drink regularly, talk to your doctor-your treatment plan may need adjusting.
How do I know if escitalopram is working for me?
Look for small, consistent improvements over time: sleeping better, having more energy, feeling less overwhelmed by daily tasks, laughing more, or having fewer panic attacks. Emotional shifts come later than physical ones. Keep a simple journal. Note changes week by week. If you’re unsure after 12 weeks, talk to your doctor about next steps.


Been on escitalopram for 10 weeks now. Week 3 was rough-insomnia and nausea like someone poured acid in my brain. But by week 6, I started noticing little things: I didn’t cancel plans with my sister. I laughed at a dumb meme. I actually got out of bed before noon. It’s not magic. It’s just… slower than you think. Stick with it. Your brain’s not broken, it’s just re-wiring.