Hyponatremia Risk Calculator
This tool helps assess your risk of developing severe hyponatremia from medications. Based on data from the article, severe cases can occur rapidly and require immediate attention. Please note that this is not a medical diagnosis.
Results will appear here after calculation
When your blood sodium drops too low, your brain starts to swell. It’s not a slow, quiet process-it can happen in hours. And one of the most common causes? Medications you’re taking for depression, high blood pressure, or seizures. Severe hyponatremia isn’t just a lab result. It’s confusion that turns to disorientation, headaches that become unbearable, and seizures that come out of nowhere. If you or someone you care about is on certain drugs, this isn’t something to ignore.
What Exactly Is Hyponatremia?
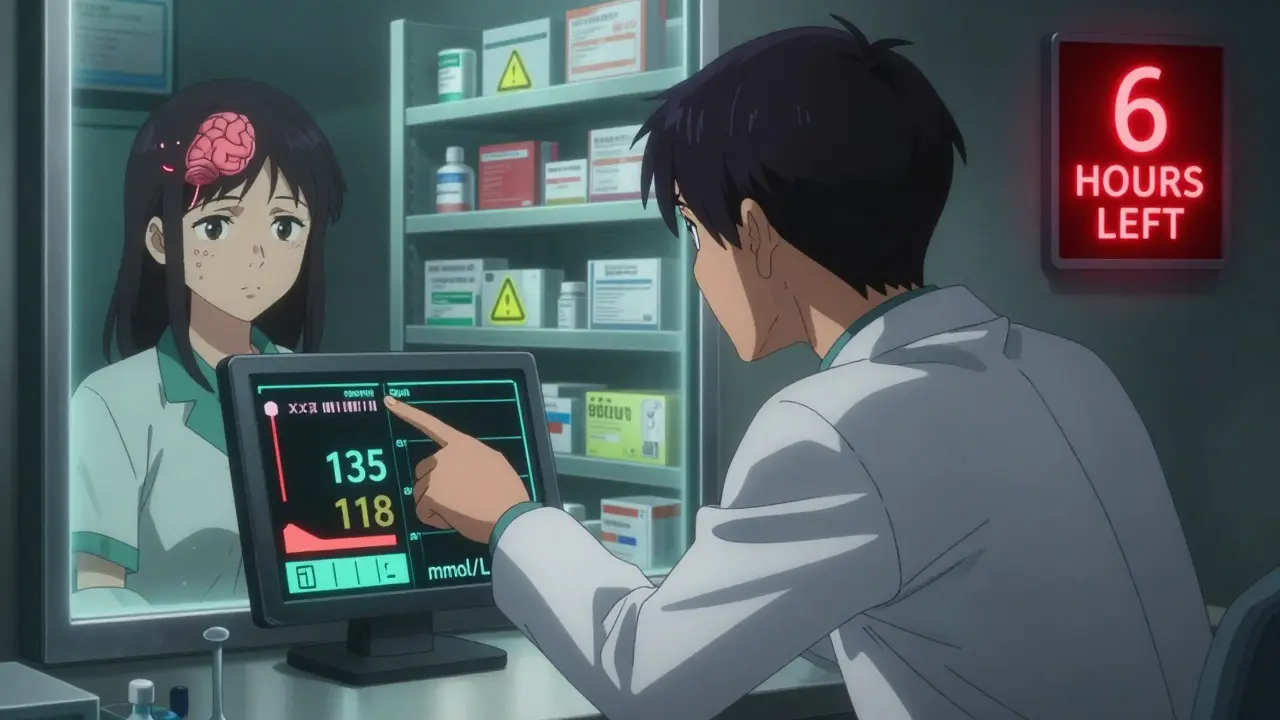
Hyponatremia means your blood sodium level is below 135 mmol/L. Severe cases fall below 120 mmol/L. Sodium isn’t just table salt-it’s a key electrolyte that controls how water moves in and out of your cells. When sodium drops, water rushes into brain cells. Your brain doesn’t have room to expand. So it swells. That’s when symptoms start.
This isn’t rare. About 1 in 5 hospitalized patients with low sodium got there because of a medication. The numbers are even higher in older adults. In people over 65, the risk jumps 2.7 times. And women are more likely to be affected than men. It’s not about being weak or unhealthy-it’s about how your body reacts to certain drugs.
Which Medications Cause It?
Not all drugs do this. But some are well-documented culprits:
- Diuretics (like hydrochlorothiazide): Responsible for nearly 3 out of 10 cases. They make you pee more, but sometimes too much water, not enough salt.
- SSRIs (sertraline, citalopram, fluoxetine): These antidepressants trigger the body to hold onto water. One nurse on Reddit described a 72-year-old patient who had a seizure just 10 days after starting sertraline. Sodium dropped 0.8 mmol/L per day-fast enough to kill brain cells.
- Antiepileptics (carbamazepine, oxcarbazepine): Carbamazepine carries a 5.3 times higher risk than non-users. A patient on Drugs.com wrote: “Hospitalized for 5 days because of low sodium from citalopram.” The same thing happens with carbamazepine.
- MAOIs, ACE inhibitors, NSAIDs, and even MDMA: These are less common but still dangerous. MDMA, for example, causes people to drink too much water during parties, but it also tricks the body into holding onto it.
The FDA now requires warning labels on 27 high-risk drugs. But only 63% of doctors actually follow the monitoring guidelines. That’s a gap between policy and practice-and it’s where people get hurt.
How Do You Know It’s Happening?
Early signs are easy to miss. They look like the flu, anxiety, or aging:
- Nausea or vomiting
- Headaches
- Loss of appetite
- Feeling tired or weak
By the time confusion sets in, it’s already serious. Sixty-eight percent of severe cases show mental changes. That’s not just “being forgetful.” It’s not knowing where you are, mixing up names, or speaking incoherently. Seizures appear in about 22% of cases when sodium drops below 115 mmol/L. Coma follows if it’s not treated.
One patient on Patient.info said her doctor called her symptoms “early dementia.” She was 68. Her sodium was 118. She spent 12 days in the hospital. That kind of misdiagnosis happens in nearly 1 in 3 emergency rooms.
Why Does This Happen So Fast?
Most people think low sodium is a slow problem. It’s not. In medication-induced cases, sodium can drop 0.5 to 1.0 mmol/L per day. That’s fast enough to trigger symptoms in under a week. The brain doesn’t have time to adapt.
Dr. Joseph Verbalis from Georgetown explains: “The brain’s adaptive response to chronic hyponatremia is significantly impaired in acute medication-induced cases.” That means your brain can’t protect itself. It’s like flooding a basement without a pump. The water rises. The walls crack. And it happens faster than you expect.
The window between confusion and seizures? As little as 6 to 8 hours. That’s why waiting for a routine check-up isn’t safe.
Who’s Most at Risk?
It’s not random. Certain people are far more likely to develop this:
- People over 65: 61% of severe cases. Their kidneys don’t regulate fluid as well. They’re often on multiple medications.
- Women: 57% of cases. Hormonal differences make them more sensitive to water retention.
- Those on multiple high-risk drugs: Taking an SSRI with a diuretic? Risk jumps dramatically.
- People with kidney or heart problems: Already struggling to balance fluids.
It’s not about being “old” or “frail.” It’s about biology. And it’s preventable-if you know what to watch for.
What Should You Do If You’re on One of These Drugs?
Don’t stop your medication. But do this:
- Ask your doctor for a baseline sodium test before starting the drug.
- Get tested again within 7 days of starting. That’s when 73% of severe cases begin.
- Check every 3-5 days during the first month, especially if you’re over 65.
- Track symptoms: Write down headaches, nausea, dizziness, or confusion. Don’t assume it’s “just side effects.”
- Know your pharmacist: One Mayo Clinic patient said their pharmacist caught a dangerous interaction before they even filled the prescription. That saved them from what happened to their sister.
There’s a tool called the Hyponatremia Algorithm from the European Hyponatremia Network. It’s used in hospitals. But you can use the same logic: If you started a new drug and now feel off, low sodium is a top suspect.
How Is It Treated?
It’s not as simple as eating more salt. In severe cases, you need hospital care. The goal isn’t to fix sodium fast-it’s to fix it safely.
Correcting sodium too quickly can cause osmotic demyelination syndrome. That’s when the brain’s protective coating gets destroyed. It leads to paralysis, locked-in syndrome, or death. That’s why doctors aim for 4-8 mmol/L correction in 24 hours. Some guidelines say 6 mmol/L max. Others allow up to 10 mmol/L with constant monitoring.
New treatments are emerging. In November 2023, the FDA approved tolvaptan (Samsca) for medication-induced hyponatremia. It helps the body get rid of excess water without losing sodium. In trials, it cut correction time by 34%.
But the best treatment? Stopping the drug-if possible. In 78% of cases, symptoms reverse once the medication is stopped. The problem? Many people can’t stop. Like someone on SSRIs for depression. Their risk of recurrence is 33%. That’s why ongoing monitoring is critical.

What’s Changing in 2026?
The landscape is shifting. The European Medicines Agency now requires pharmacists to give sodium monitoring instructions when dispensing high-risk drugs. That’s huge. It puts the responsibility where it should be-not just on doctors, but on the whole care team.
And AI is stepping in. Mayo Clinic is testing an algorithm that predicts hyponatremia risk 72 hours before symptoms show. It scans your EHR-meds, lab results, age, weight-and flags danger. Accuracy? 87%. That’s not science fiction. It’s happening now.
But until these tools are everywhere, you have to be your own advocate.
Why This Matters More Than Ever
Medication-induced hyponatremia costs the U.S. health system $473 million a year. Hospitalizations are rising. SSRI prescriptions have gone up 18.7% since 2018. The population is aging. By 2028, cases could jump 22%.
But here’s the good news: if caught early, 92% of people recover fully. If treatment is delayed past 48 hours, that drops to 67%. That’s not just a statistic. That’s a person. A parent. A grandparent. Someone who thought their headache was just stress.
The system isn’t perfect. But you don’t have to wait for it to fix itself. Ask for a test. Track your symptoms. Speak up. Your sodium level isn’t just a number. It’s your brain’s lifeline.
What to Do If You Think You Have It
If you’re on a high-risk drug and suddenly feel confused, nauseous, or have a seizure:
- Don’t wait for your next appointment.
- Go to an ER or call emergency services.
- Bring a list of all your medications-including over-the-counter and supplements.
- Ask: “Could this be low sodium from my meds?”
There’s no harm in asking. But the cost of not asking? It’s irreversible.


Wow, this is one of those posts that makes you want to call your grandma and ask if she’s been feeling ‘off’ lately. I had no idea SSRIs could do this-my aunt was on sertraline for years and they just called her ‘forgetful.’ Turns out her sodium was 119. She’s fine now, but it took a trip to the ER to figure it out. Please, if you’re on meds and feel weird, get tested. It’s not anxiety, it’s biology.