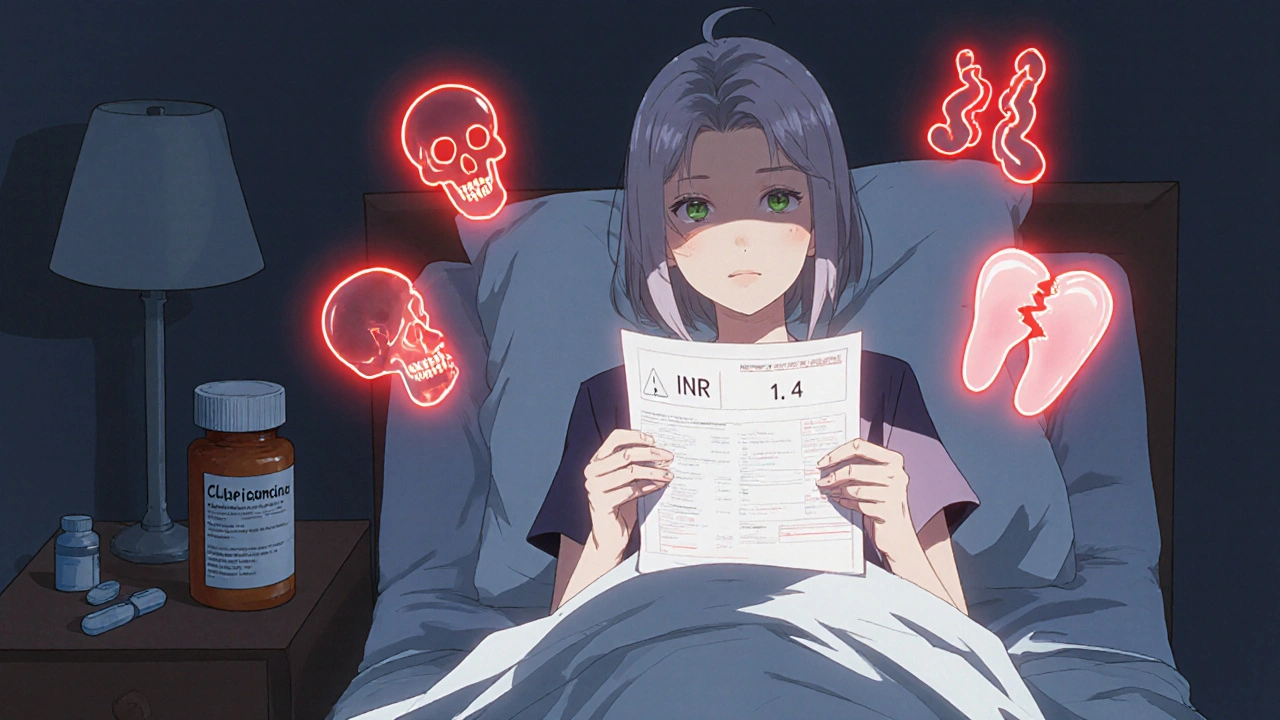
INR Increase: What It Means, Why It Happens, and What to Do
When your INR increase, International Normalized Ratio is a standardized measure of how long it takes your blood to clot. Also known as prothrombin time ratio, it’s a critical number for people taking blood thinners like warfarin. A higher INR means your blood is thinner—and that’s not always a bad thing, but it can become dangerous if it goes too high.
Most people on warfarin aim for an INR between 2.0 and 3.0. If your INR climbs above 4.0, your risk of bleeding goes up sharply—think nosebleeds that won’t stop, bruising without injury, or worse, internal bleeding. But why does this happen? It’s rarely just one thing. Warfarin, a vitamin K antagonist used to prevent dangerous clots in conditions like atrial fibrillation or deep vein thrombosis interacts with food, other drugs, and even your liver’s ability to process it. Eating more leafy greens? That’s vitamin K, and it can drop your INR. Got sick with the flu? Your liver slows down, and your INR spikes. Started a new antibiotic? Some, like cefaclor or tinidazole, can interfere with warfarin metabolism and push your INR up unexpectedly.
It’s not just about the medication. Anticoagulants, drugs designed to reduce the risk of stroke or clotting by slowing down the blood’s clotting process like warfarin require constant monitoring. Even small changes in your routine—missing a dose, drinking more alcohol, starting a new supplement like fish oil or ginkgo—can throw your INR off. That’s why regular blood tests aren’t optional. They’re your safety net. If your INR is rising, your doctor might pause your dose, give you vitamin K, or adjust your schedule. Never change your dose on your own, even if you feel fine. Bleeding doesn’t always come with warning signs.
Some people worry that an INR increase means they’re doing something wrong. It doesn’t. Life happens. Illnesses change how your body handles drugs. New medications get added. Your diet shifts. Even stress can play a role. The key isn’t perfection—it’s awareness. Keep a simple log: what you ate, what meds you took, any symptoms. Bring it to your next appointment. That’s how you turn random spikes into predictable patterns.
Below, you’ll find real-world guides on how medications interact, how to track your treatment, and what to do when things don’t go as planned. Whether you’re managing warfarin, dealing with a recent INR spike, or just trying to understand why your doctor keeps ordering blood tests, these posts give you the facts without the fluff. No jargon. No guesswork. Just what you need to stay safe and in control.
Warfarin and Antibiotics: How Common Antibiotics Can Spike Your INR Risk
Warfarin and certain antibiotics can dangerously raise INR levels, increasing bleeding risk. Learn which antibiotics are most risky, how to monitor your INR, and what to do if your levels spike.
More Detail