Warfarin and Antibiotics: What You Need to Know About Dangerous Interactions
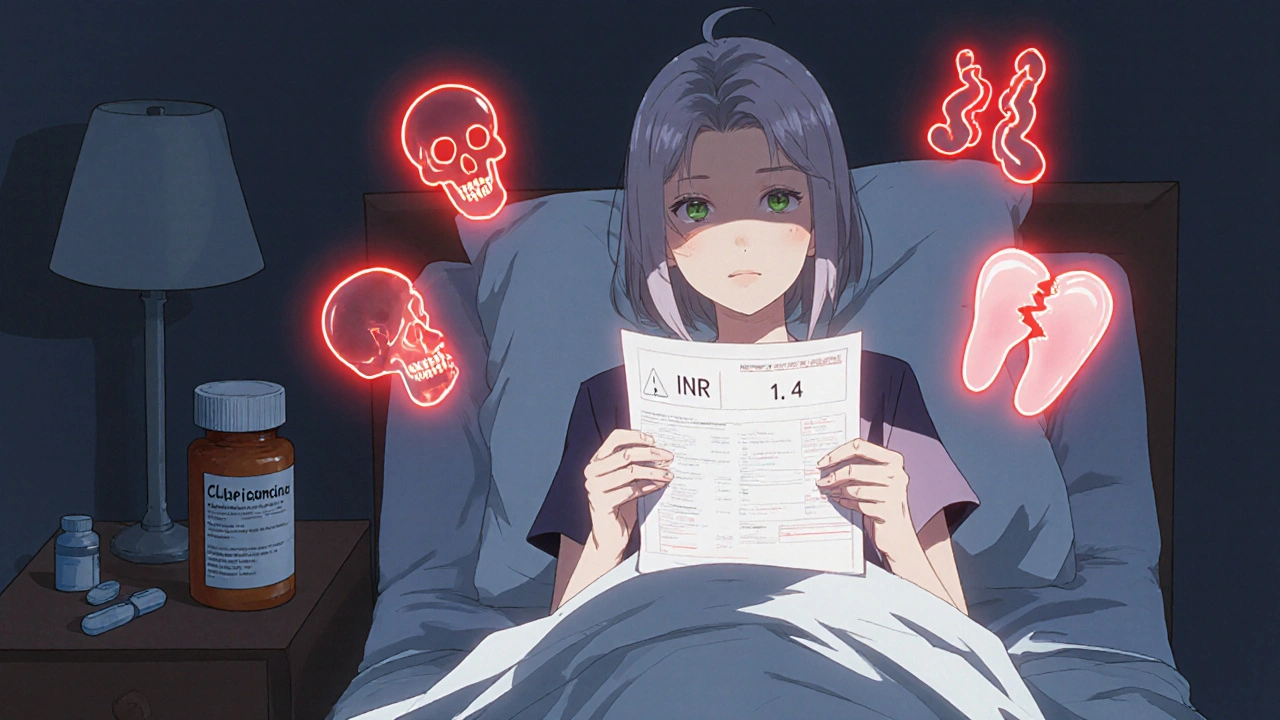
When you take warfarin, a blood thinner used to prevent clots in people with atrial fibrillation, artificial heart valves, or a history of deep vein thrombosis. Also known as Coumadin, it works by blocking vitamin K, which your body needs to make clotting factors. But if you start an antibiotic, a medicine used to kill or slow the growth of bacteria causing infections like pneumonia, urinary tract infections, or skin abscesses, things can go wrong fast. Some antibiotics don’t just treat your infection—they change how warfarin works in your body, making your blood too thin or not thin enough.
It’s not all antibiotics. Some, like trimethoprim-sulfamethoxazole (Bactrim), ciprofloxacin (Cipro), and metronidazole (Flagyl), are known to boost warfarin’s effect. That means your INR—your blood’s clotting time—can spike overnight. You might not feel anything at first, but then you notice bruising without bumping into anything, or a nosebleed that won’t stop. Other antibiotics, like rifampin, do the opposite: they make warfarin less effective, raising your risk of a clot. This isn’t theoretical. Studies show patients on warfarin who start these antibiotics are up to 5 times more likely to have a dangerous bleed.
Your doctor doesn’t always catch this. Many assume if you’ve been on warfarin for years, you’re fine. But changes happen fast. A 5-day course of an antibiotic can throw your INR out of range by day 3. That’s why you need to tell every provider—your dentist, urgent care, even your pharmacist—that you’re on warfarin. And if you’re prescribed a new antibiotic, ask: "Will this affect my blood thinner?" If they don’t know, ask for a quick INR check before you start it. Some pharmacies even flag these interactions automatically.
You’re not alone in this. Millions take warfarin. Thousands get antibiotics every year. The overlap is huge. But the real problem isn’t the drugs—it’s the silence around them. People don’t know to watch for signs. They don’t know to test sooner. They assume their doctor is monitoring everything. But your safety depends on you knowing what to look for: unusual bleeding, dark stools, headaches that won’t quit, swelling in your legs. And you need to act fast.
Below, you’ll find real-world guides that break down exactly how these interactions work, which antibiotics are safest, how to track your INR at home, and what to do when your doctor isn’t sure. These aren’t theory pieces. They’re written by people who’ve been through it—patients and clinicians who’ve seen the mistakes, fixed them, and learned how to stay safe. You don’t need to guess. You just need to know what to ask, what to watch, and when to act.
Warfarin and Antibiotics: How Common Antibiotics Can Spike Your INR Risk
Warfarin and certain antibiotics can dangerously raise INR levels, increasing bleeding risk. Learn which antibiotics are most risky, how to monitor your INR, and what to do if your levels spike.
More Detail