It’s easy to assume that if you’re taking medications as prescribed, you’re safe. But what if your blood pressure pill starts making you dizzy when you add a new over-the-counter cold medicine? Or what if your antidepressant causes a racing heart after you take ibuprofen for a headache? These aren’t just bad luck-they could be drug interactions, and they can turn dangerous fast.
Drug interactions happen when one substance changes how another works in your body. This could be another prescription, an OTC pill, a supplement, even grapefruit juice or alcohol. The result? A drug might stop working, become too strong, or trigger side effects you’ve never felt before. According to the CDC, over 1.3 million emergency room visits in the U.S. each year are caused by these kinds of reactions. And the worst part? Most people don’t realize what’s happening until it’s too late.
When to Call 911 Right Away
Some drug interactions are medical emergencies. If you or someone else experiences any of these symptoms, don’t wait. Call emergency services immediately.
- Difficulty breathing or oxygen levels below 90%-This is a sign your airway is closing or your lungs are failing. It can happen in severe allergic reactions to antibiotics, NSAIDs, or even certain painkillers.
- Swelling of the face, lips, tongue, or throat-This is angioedema. It can block your airway in minutes. People on ACE inhibitors, penicillin, or sulfa drugs are at higher risk.
- Systolic blood pressure below 90 with a heart rate over 120-This means your body is going into shock. It’s common in anaphylaxis from drugs like penicillin, chemotherapy, or contrast dyes used in scans.
- Seizures lasting more than 2 minutes-This can happen with overdose or interaction of drugs like tramadol, bupropion, or even some antibiotics when mixed with other stimulants.
- Temperature above 41.1°C (106°F), rigid muscles, and uncontrollable agitation-This is serotonin syndrome, often triggered when SSRIs like fluoxetine or sertraline are mixed with other serotonergic drugs like tramadol, dextromethorphan, or even St. John’s Wort. About 1-2% of people on multiple serotonergic drugs develop this. It kills if untreated.
- High fever over 40°C, dark urine, and extreme muscle pain-This could be neuroleptic malignant syndrome, a rare but deadly reaction to antipsychotics like haloperidol or risperidone, especially when combined with other drugs that affect dopamine.
These aren’t "wait and see" situations. In serotonin syndrome, symptoms can escalate from mild shivering to full organ failure in under 24 hours. A 2022 study in Emergency Medicine Cases found that patients who waited more than 6 hours to seek help had a 60% higher chance of needing ICU care.
When to See a Doctor Within 24 Hours
If you’re not in immediate danger but something feels deeply wrong, don’t brush it off. These symptoms need medical attention within a day.
- A widespread rash covering more than 30% of your skin-This could be DRESS syndrome, a severe delayed reaction to anticonvulsants like carbamazepine, antibiotics like sulfonamides, or allopurinol. It often comes with fever, swollen lymph nodes, and organ damage.
- Unexplained fever above 38.5°C (101.3°F) lasting more than 48 hours-If you’ve started a new antibiotic, antiviral, or seizure medication, this could be serum sickness or another immune reaction. It’s not just a cold.
- Unusual bruising, bleeding gums, or nosebleeds-A platelet count below 100,000/μL means your blood can’t clot properly. This can happen with heparin, quinolone antibiotics, or even some herbal supplements like ginkgo biloba.
- Yellow skin or eyes, dark urine, or persistent nausea-ALT liver enzyme levels over 120 U/L signal drug-induced liver injury. This is common with statins, acetaminophen (especially when mixed with alcohol), and some TB medications.
- Urine output below 0.5 mL per kg per hour for 6+ hours-This means your kidneys are shutting down. It can happen with NSAIDs, certain antibiotics, or contrast dyes used in imaging tests.
Many people think, "I’ve felt this way before," or "It’ll pass." But in a 2022 survey by the National Community Pharmacists Association, 58% of patients waited over 12 hours before calling their doctor-even after experiencing severe dizziness or vomiting. By then, damage can be done.
Who’s at Highest Risk?
You’re not equally likely to have a bad interaction. Risk goes up if:
- You take five or more medications daily-The Journal of the American Geriatrics Society found a 57% chance of a major interaction in people on five or more drugs.
- You’re over 65-Older adults are more likely to have multiple conditions and take more meds. In the U.S., 45% of adults over 65 are on five or more prescriptions.
- You take drugs with a narrow therapeutic index-These are medications where a small change in blood level can be dangerous. Examples: warfarin (blood thinner), digoxin (heart medication), phenytoin (seizure drug), and lithium (mood stabilizer). A 20% change in concentration can cause overdose or treatment failure.
- You use herbal supplements-St. John’s Wort, ginkgo, garlic, and echinacea interact with dozens of prescription drugs. The NIH reports these account for 18% of serious interactions.
One real case from Reddit: a 72-year-old man on warfarin started taking a turmeric supplement for joint pain. His INR (blood clotting measure) shot up to 12. He ended up in the ER with internal bleeding. He had no idea turmeric thins the blood.
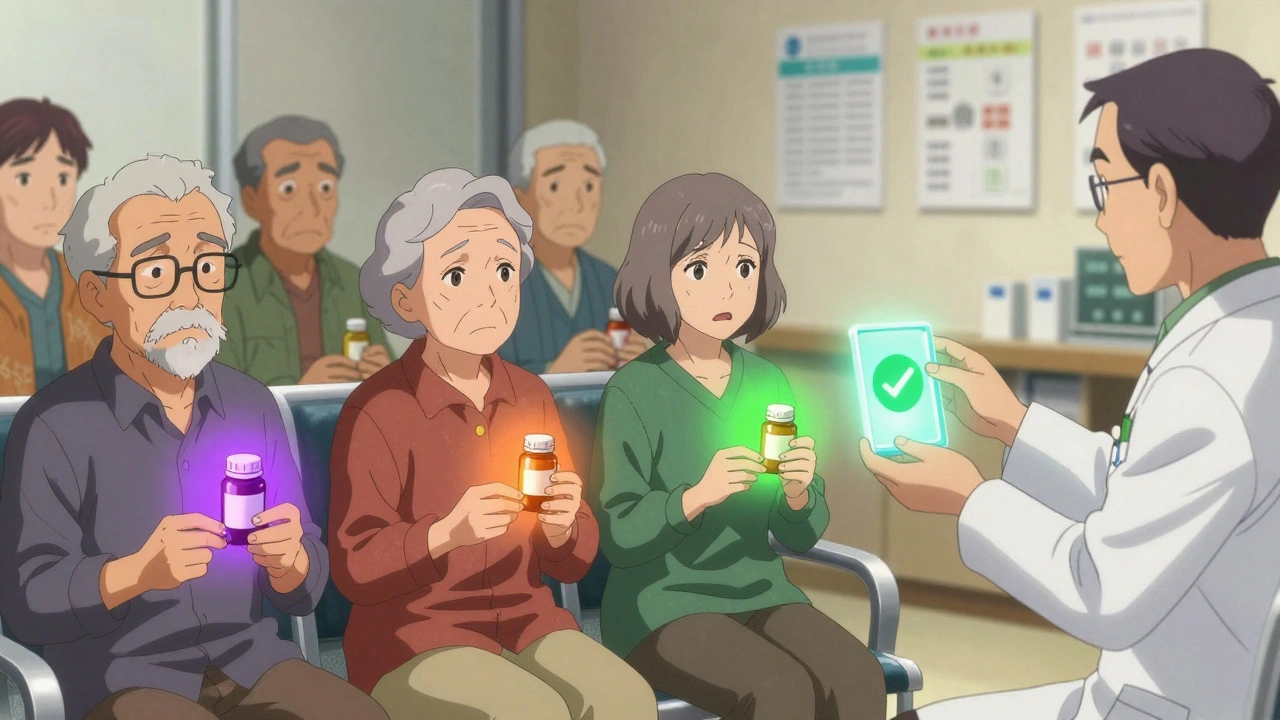
What You Can Do Before It Gets Worse
Prevention is always better than emergency care. Here’s how to protect yourself:
- Keep a full list of everything you take-Prescriptions, OTC meds, vitamins, supplements, and even herbal teas. Write down the dose and how often you take it.
- Use a drug interaction checker-Drugs.com has a free tool that checks over 24,000 medications and 500,000 interactions. It includes supplements. Always enter everything-even the "harmless" ones.
- Ask your pharmacist every time-They’re trained to spot interactions. If you pick up a new prescription, ask: "Could this interact with anything else I’m taking?"
- Use the STOP protocol-If you suspect a reaction: Stop the new medication, Telephone your provider, Observe symptoms, Present all medication containers at your appointment.
Studies show that patients who call poison control within one hour of noticing symptoms are 89% more likely to avoid the ER. The American Association of Poison Control Centers handled 2.1 million exposure calls in 2022-and 65% of those were managed without hospital visits.
Why Doctors Miss These Too
It’s not just patients. Even doctors get overwhelmed. A 2022 survey found that 47% of primary care physicians override interaction warnings because they get too many alerts. This is called "alert fatigue." Electronic health records pop up warnings for every possible interaction-even ones that are unlikely or harmless.
But tools are improving. The Liverpool Drug Interaction Group checker, used in HIV clinics, has 94% accuracy. AI systems like IBM Watson Drug Insights can predict new interactions with 89% accuracy. The FDA’s Sentinel Initiative now tracks 300 million patient records to catch emerging risks.
The bottom line? You can’t rely on technology alone. You have to be your own advocate.
What to Bring to Your Appointment
If you go to the doctor because of a suspected interaction, don’t just describe your symptoms. Bring:
- All medication bottles-Including vitamins, supplements, and herbal products.
- A list of when you started each one.
- When the symptoms started and how they’ve changed.
- Any recent changes in diet, alcohol use, or sleep.
This gives your provider the full picture. Without it, they’re guessing. And guessing with drug interactions can cost lives.
Drug interactions don’t always cause dramatic symptoms. Sometimes, they just make you feel "off." That’s often the first warning. If you’re taking more than one medication and something feels wrong-trust it. Don’t wait for it to get worse.
Can over-the-counter drugs cause serious interactions?
Yes. Common OTC drugs like ibuprofen, naproxen, antacids, and cold medicines can interact with prescription drugs. For example, mixing ibuprofen with warfarin increases bleeding risk. Taking antacids with antibiotics like ciprofloxacin can make the antibiotic ineffective. Even acetaminophen (Tylenol) can damage your liver if taken with alcohol or certain seizure meds.
Are herbal supplements safe if they’re "natural"?
No. "Natural" doesn’t mean safe. St. John’s Wort can make birth control, antidepressants, and blood thinners stop working. Garlic and ginkgo can increase bleeding risk before surgery. Echinacea can interfere with immune-suppressing drugs. The NIH says herbal supplements cause 18% of serious drug interactions.
Can food cause drug interactions?
Absolutely. Grapefruit juice affects over 85 medications, including statins, blood pressure drugs, and immunosuppressants. It can make them too strong, leading to overdose. Dairy products can block absorption of antibiotics like tetracycline. High-fiber foods can reduce the effect of some thyroid meds. Always check the label or ask your pharmacist.
What should I do if I think I’m having a drug interaction?
If symptoms are severe-trouble breathing, swelling, chest pain, seizures, or high fever-call 911 immediately. For milder but concerning symptoms like rash, fever, dizziness, or unusual bleeding, call your doctor or poison control (1-800-222-1222 in the U.S.). Don’t stop your meds unless told to. Bring all your medication bottles to your appointment.
How common are drug interactions?
Very. About 30% of hospitalized patients experience an adverse drug reaction, and 40% of those are preventable. The average person taking five or more medications has a 57% chance of a major interaction. With polypharmacy rising, especially in older adults, this is a growing public health issue.
Can I check for interactions myself?
Yes. Use trusted tools like Drugs.com’s interaction checker, which includes prescription, OTC, and supplement data. You can also ask your pharmacist to run a check when you pick up a new prescription. But don’t rely on Google searches or social media advice. Only use verified medical sources.
Drug interactions aren’t rare accidents-they’re predictable risks. The more meds you take, the more you need to stay alert. Your life could depend on recognizing the signs early.


So let me get this straight - you're telling me that my grapefruit juice and my blood pressure med are having a secret affair that could kill me? And I thought my ex was toxic. 🤯 I just drank half a gallon this morning. Guess I'm buying orange juice now. RIP my breakfast routine.