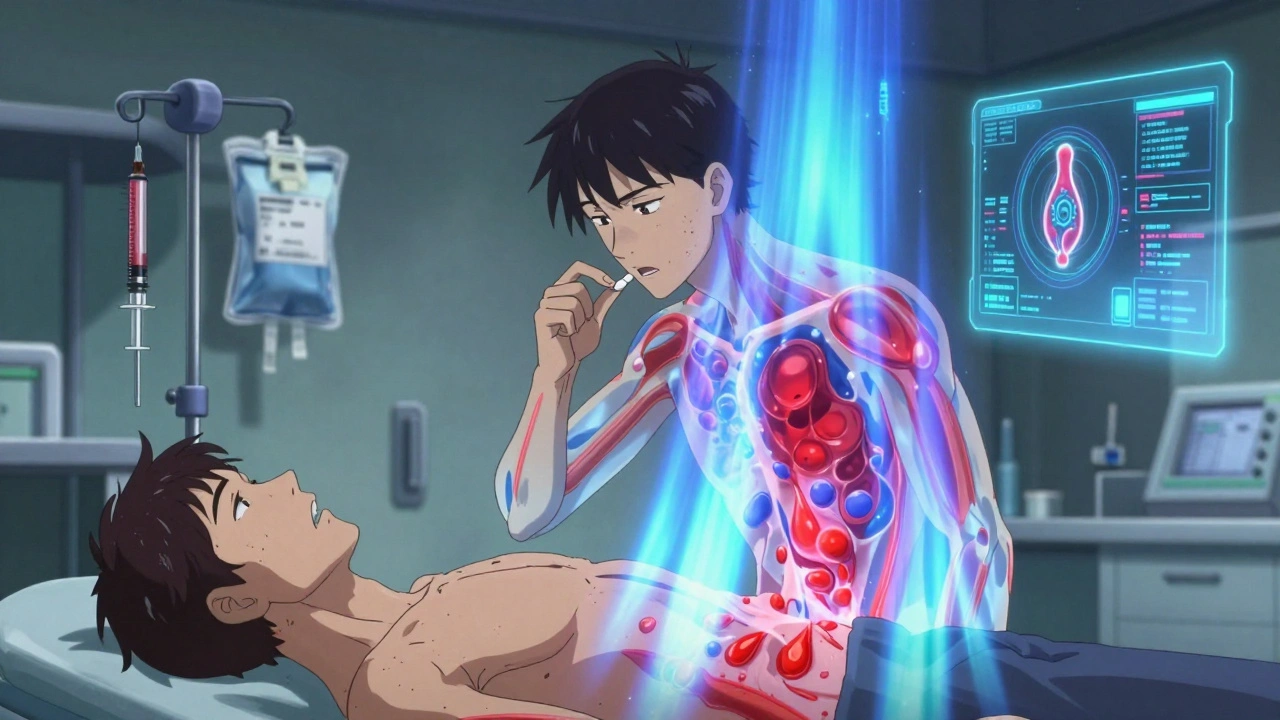
When your kidneys start to fail, they don’t just stop filtering waste-they also stop making a key hormone called erythropoietin. Without it, your bone marrow doesn’t get the signal to produce enough red blood cells. The result? Anemia. It’s not just fatigue. It’s gasping for air after walking to the mailbox, feeling dizzy standing up, or watching your grandchildren play but being too tired to join in. For people with chronic kidney disease (CKD), this isn’t rare-it’s expected. About 90% of those on dialysis have anemia. But here’s the good news: we know exactly how to fix it. And it starts with two things: erythropoietin and iron.
Why Kidney Disease Causes Anemia
Your kidneys make erythropoietin, a hormone that tells your body to build red blood cells. When kidney function drops below 30%, that production plummets. But it’s not just a lack of hormone. Inflammation from kidney disease also blocks iron from reaching your bone marrow. Even if you have iron in your body, it’s locked away-like a key stuck in a rusted lock. This is called functional iron deficiency. And if you’re taking oral iron pills, they barely work because your gut can’t absorb them properly when inflammation is high.
So anemia in CKD isn’t just low hemoglobin. It’s a mix of three problems: not enough erythropoietin, iron that won’t move, and inflammation that makes both worse. That’s why treating it isn’t as simple as taking a vitamin. You need the right tools, at the right time.
Erythropoietin Therapy: The Hormone Replacement
Back in 1989, doctors got a game-changer: synthetic erythropoietin. It was the first time we could replace what damaged kidneys couldn’t make. Today, we have several versions-epoetin alfa, darbepoetin alfa, and newer biosimilars like Retacrit. They’re given either as shots under the skin (for non-dialysis patients) or through the IV line during dialysis.
These drugs work fast. Most people see their hemoglobin rise by 1 to 2 grams per deciliter in just 2 to 6 weeks. But here’s the catch: you can’t just push hemoglobin as high as possible. Studies like the TREAT trial showed that pushing hemoglobin above 11.5 g/dL increases stroke risk by 32%. Too much can also raise blood pressure, cause clots, and even raise the chance of heart attacks.
That’s why current guidelines, like the 2025 KDIGO draft, say: aim for 10 to 11.5 g/dL. Not 12. Not 13. Just enough to feel better, not enough to put you at risk. And it’s not one-size-fits-all. A 70-year-old with heart disease might do best at 10 g/dL. A younger, active person might feel better at 11. The goal isn’t a number-it’s your quality of life.
Iron Therapy: The Missing Piece
Here’s the truth most people don’t know: if your iron levels are low, erythropoietin won’t work well. You can give all the hormone you want, but without iron, your body can’t make red blood cells. That’s why iron therapy isn’t optional-it’s the foundation.
Oral iron? It’s mostly useless in CKD. Your gut absorbs only 30-40% of it because of hepcidin, a protein that shuts down iron absorption during inflammation. That’s why IV iron is the standard. Drugs like iron sucrose (Venofer) or ferric carboxymaltose go straight into your bloodstream. One dose of 200 mg can boost hemoglobin by 0.5 g/dL. A full course of 1,000 mg can raise it by 1.5 g/dL in just four weeks.
But how do you know when to give it? The numbers matter:
- Ferritin below 100 mcg/L? You have absolute iron deficiency. Start IV iron now.
- Ferritin 100-500 mcg/L with transferrin saturation (TSAT) under 20-30%? That’s functional deficiency. Still need IV iron.
- Ferritin over 700 mcg/L or TSAT over 40%? Hold off. Too much iron can damage your liver and heart.
For hemodialysis patients, many centers give 400 mg of IV iron every month-whether they’re “deficient” or not. Why? Because inflammation constantly pulls iron out of circulation. It’s like trying to fill a bucket with a hole in the bottom. You have to keep pouring.

What Happens If You Don’t Treat It?
Left untreated, anemia in CKD doesn’t just make you tired. It strains your heart. Your heart has to pump harder to deliver enough oxygen. Over time, that leads to left ventricular hypertrophy-a thickening of the heart muscle. That’s a direct path to heart failure.
People with untreated anemia are also more likely to need blood transfusions. And transfusions? They carry risks: infections, immune reactions, and iron overload. Plus, they don’t fix the root problem. They’re a band-aid, not a cure.
And then there’s the mental toll. Patients report feeling like they’re living in slow motion. One woman on a kidney forum said, “I used to garden every weekend. Now I can’t even carry my laundry up the stairs.” That’s not normal aging. That’s treatable anemia.
The New Frontier: HIF-PHIs
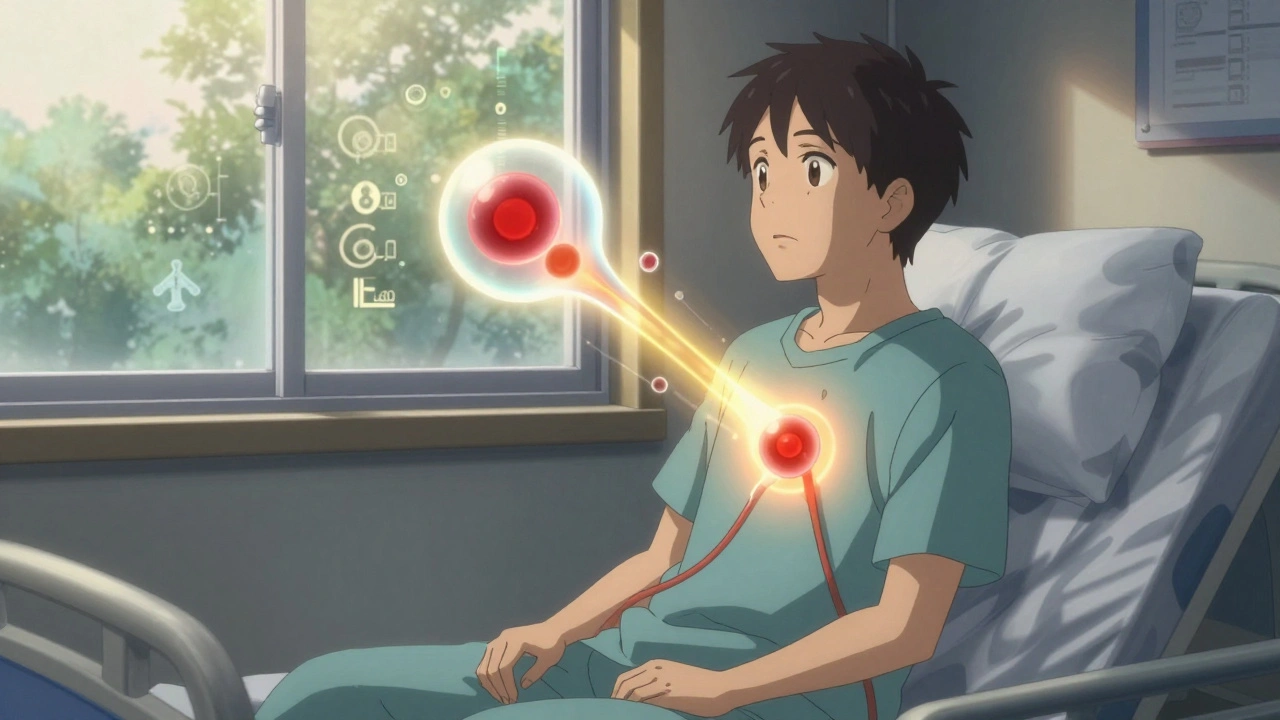
For years, we had two tools: shots of erythropoietin and IV iron. Now, there’s a third: oral pills called HIF-PHIs. Roxadustat, approved in the U.S. in December 2023, works differently. Instead of replacing erythropoietin, it tricks your body into making more of its own. It also helps move iron around-making it useful even when inflammation is high.
The benefits? No injections. Better iron use. And early data suggests it might be gentler on the heart than traditional ESAs. But it’s not perfect. The FDA put a hold on these drugs from 2018 to 2020 over concerns about tumor growth in cancer patients. That’s why they’re not recommended for people with active cancer.
Right now, HIF-PHIs are expensive. But they’re growing fast. By 2028, they could make up a $3.5 billion market. For patients tired of needles, they’re a lifeline.
How Treatment Actually Works in Real Life
Here’s how it plays out in the clinic:
- Check hemoglobin. If it’s below 12 g/dL for women or 13 g/dL for men, test ferritin and TSAT.
- If ferritin is under 500 mcg/L and TSAT under 30%, start IV iron-even if you’re not on dialysis yet.
- Wait 4-8 weeks. Recheck hemoglobin. If it’s still below 10 g/dL, start an ESA.
- Adjust ESA dose slowly. Increase by 25% every 4 weeks if hemoglobin rises too slowly. Cut it if it goes up too fast.
- Monitor every month. Blood pressure, hemoglobin, ferritin, TSAT. No skipping visits.
And if hemoglobin doesn’t rise after 12 weeks of full-dose ESA and iron? That’s ESA hyporesponsiveness. It could mean hidden inflammation, aluminum toxicity, or even a vitamin B12 deficiency. Time to dig deeper.
What Patients Really Experience
People who get treated often say the same thing: “I feel like myself again.” One 62-year-old man with diabetes and CKD went from 8.2 to 10.5 g/dL in eight weeks. He started walking his dog again. He cooked dinner for his wife. He didn’t nap after lunch.
But side effects are real. About 32% of patients report worse high blood pressure after starting ESAs. Some need new meds. About 45% of those getting IV iron say they taste metal in their mouth. A quarter feel flu-like for a day after the infusion. Injection sites can get red or sore.
And the cost? In the U.S., ESAs still make up 75% of the anemia treatment market. But with Medicare bundling since 2011, hospitals are pressured to use less. That’s why many now start with IV iron first-and use ESAs only when needed.
Where the Guidelines Differ
Not every country agrees. The U.S. KDOQI guidelines from 2007 say aim for 11-12 g/dL. But KDIGO (the global standard) says 10-11.5 g/dL. Why the difference? Because U.S. studies were older. Newer trials, reviewed up to April 2023, show higher targets increase risk.
And in Europe, many centers give IV iron every month, no questions asked. In the U.S., some still wait for ferritin to drop below 100. That’s outdated. The evidence now supports proactive iron use-even in patients who aren’t “deficient” by old standards.
The bottom line? The best care isn’t about following a rulebook. It’s about watching the patient. Are they tired? Are they getting worse? Are they improving? That’s what matters more than a number on a lab report.
What’s Next?
The future is personalization. Researchers at Mayo Clinic are testing AI algorithms that predict exactly how much ESA or iron a patient needs-based on their weight, age, inflammation levels, and past response. Early results show a 22% drop in dose errors.
And new drugs are coming. Minihepcidins could unlock iron trapped by inflammation. New ESAs with longer half-lives might mean monthly shots instead of weekly. The goal isn’t just to treat anemia. It’s to restore energy, independence, and life.
For people with kidney disease, anemia isn’t a side effect. It’s a core part of the disease. And now, we have the tools to fight it-smartly, safely, and one patient at a time.
Can I treat anemia in kidney disease with iron pills alone?
No. Oral iron is rarely effective in chronic kidney disease because inflammation blocks absorption. Even high doses won’t raise iron levels enough to support red blood cell production. IV iron is the standard because it bypasses the gut and delivers iron directly into the bloodstream.
What’s the ideal hemoglobin target for someone with kidney disease?
The current global standard (KDIGO 2025 draft) recommends keeping hemoglobin between 10 and 11.5 g/dL. Going higher increases the risk of stroke, heart attack, and blood clots. The goal isn’t to reach a number-it’s to feel better without adding health risks.
How long does it take for iron therapy to work?
IV iron can raise hemoglobin by about 0.5 g/dL within two weeks. A full course of 1,000 mg typically boosts levels by 1.5 g/dL in four weeks. Oral iron, even if absorbed, takes 8-12 weeks for minimal improvement-and often fails completely in CKD.
Can I stop erythropoietin therapy once my hemoglobin improves?
Usually not. Kidneys with chronic damage won’t start making erythropoietin again. Stopping the drug will cause hemoglobin to drop back down within weeks. Therapy is typically lifelong unless you get a kidney transplant.
Are HIF-PHIs better than traditional erythropoietin injections?
They offer advantages: oral dosing, better iron utilization, and possibly fewer cardiovascular side effects. But they’re not for everyone-especially if you have cancer or are at high risk for tumors. They’re also more expensive. For now, they’re a valuable alternative, not a replacement.
What if my anemia doesn’t improve with treatment?
If hemoglobin doesn’t rise after 12 weeks of full-dose ESA and IV iron, you may have ESA hyporesponsiveness. Causes include ongoing inflammation, aluminum toxicity, vitamin deficiencies, or poor adherence. Your doctor will need to run more tests to find the hidden cause.
Managing anemia in kidney disease isn’t about one drug or one number. It’s about balancing safety, effectiveness, and your daily life. With the right approach, you don’t have to accept fatigue as part of the diagnosis. You can reclaim your energy-and your life.

Man, this post hit different. I’ve been on dialysis for 5 years, and honestly? The first time I got IV iron, I thought I was dreaming. Walked to the mailbox without stopping. Held my granddaughter without my chest feeling like a brick. It’s not magic-it’s science, and it works. Thanks for laying it out so clear.