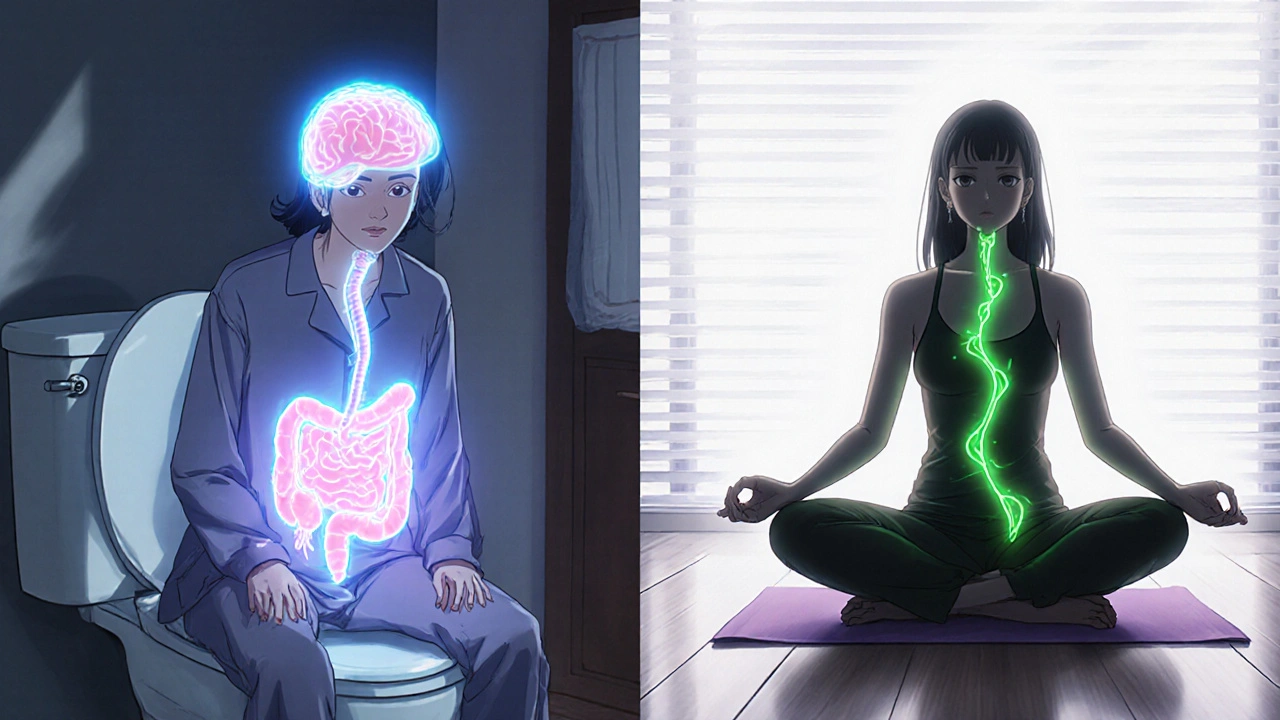
If you’ve been dealing with constant bloating, cramps, or unpredictable bathroom trips, you’re not alone. Around 1 in 7 people worldwide live with irritable bowel syndrome, or IBS. It’s not just a "sensitive stomach"-it’s a real, diagnosable condition that can mess with your daily life. Unlike Crohn’s or colitis, IBS doesn’t damage your gut lining, but it can make you feel like your insides are on fire, swollen, or stuck. The good news? You can manage it. This isn’t about finding a magic cure-it’s about understanding what’s going on inside you and what actually works to feel better.
What Does IBS Actually Feel Like?
IBS symptoms vary, but they’re usually tied to your bowel habits and abdominal discomfort. Most people feel pain or cramping that gets worse after eating and improves after going to the bathroom. Bloating is another big one-your stomach might look like you’re five months pregnant, even if you just had a light salad. You might also notice changes in your stool: either loose, watery stools (diarrhea), hard, lumpy stools (constipation), or switching back and forth between the two.Some people get mucus in their stool, feel like they haven’t fully emptied their bowels, or deal with excessive gas. These aren’t "just in your head"-they’re physical reactions tied to how your gut and brain communicate. About 7 in 10 people with IBS also report symptoms outside the gut: a lump in the throat, acid reflux, nausea, or even chest pain that feels like a heart issue but isn’t.
Doctors classify IBS into three main types based on your dominant bowel pattern:
- IBS-D (diarrhea-predominant): About 40% of cases. You’re rushing to the bathroom often, especially after meals.
- IBS-C (constipation-predominant): Around 35%. You’re straining, feeling backed up, and going less than three times a week.
- IBS-M (mixed): Roughly 25%. You alternate between diarrhea and constipation-sometimes even in the same day.
Knowing your subtype helps guide treatment. If you’re always running to the toilet, treating you like someone who’s constipated won’t help. It’s like trying to fix a leaky faucet by tightening it-wrong tool for the job.
How Do You Know It’s IBS-and Not Something Else?
There’s no single test for IBS. Doctors diagnose it by ruling out other conditions and matching your symptoms to the Rome IV criteria: abdominal pain at least once a week for the last three months, with symptoms starting at least six months ago, plus changes in bowel habits.But here’s the catch: if you’re over 45 and suddenly start having digestive issues, or if you’re losing weight without trying, having blood in your stool, or anemia, you need more tests. These are red flags that could point to colon cancer, celiac disease, or inflammatory bowel disease. Blood tests, stool tests for inflammation (like calprotectin), and sometimes a colonoscopy are used to make sure it’s not something more serious.
Many people wait years to get diagnosed. On Reddit’s IBS community, the average time from first symptoms to diagnosis is over six years. That’s because doctors often assume it’s stress or a "bad diet." But IBS is real, and it’s not your fault.
What Makes IBS Symptoms Worse?
Triggers are different for everyone, but some patterns show up again and again. About 70% of people with IBS say certain foods make their symptoms flare. The biggest culprits? High-FODMAP foods-things like onions, garlic, beans, apples, wheat, and dairy. These are short-chain carbs that ferment in your gut and cause gas, bloating, and pain. You don’t have to cut them out forever, but identifying which ones hit you is key.Stress is another major trigger. If you’ve ever felt your stomach twist before a big presentation or during a fight, you’ve felt the gut-brain connection. Around 60-80% of people report worse symptoms during stressful times. It’s not psychological-it’s biological. Your gut has its own nervous system, and when you’re stressed, it sends signals that speed up or slow down digestion.
For women, hormones play a big role. Around two-thirds of IBS patients are female, and many say their symptoms spike right before or during their period. Estrogen and progesterone levels affect gut motility, which is why IBS often starts or worsens during puberty, pregnancy, or perimenopause.
Antibiotics can also trigger IBS. About 1 in 4 people develop symptoms after a course of antibiotics. That’s because they wipe out good bacteria in your gut, throwing off the balance. It’s why some people say they "never had digestive issues until after that round of amoxicillin."
Medications That Actually Work
There’s no one-size-fits-all pill for IBS, but several medications have been proven to help based on your subtype.For IBS-D (diarrhea):
- Loperamide (Imodium): Available over the counter. Helps slow down bowel movements. Works for about 60% of people, but doesn’t touch the pain or bloating.
- Rifaximin (Xifaxan): An antibiotic that targets gut bacteria without affecting the rest of your body. Taken for 14 days, it reduces bloating and diarrhea in about half of users.
- Eluxadoline (Viberzi): Approved in 2015. It tightens the gut muscles and reduces nerve signals causing pain and diarrhea. Works for 40-50% of people, but isn’t safe if you don’t have a gallbladder or have a history of pancreatitis.
For IBS-C (constipation):
- Linaclotide (Linzess): Taken daily, it increases fluid in the intestines to soften stool and reduce pain. About 30-40% of people get at least three full bowel movements a week.
- Plecanatide (Trulance): Similar to linzess, but with fewer side effects like diarrhea. Works well for those who can’t tolerate linzess.
- Lubiprostone (Amitiza): A chloride channel activator that pulls water into the gut. Helps about a quarter of users, but can cause nausea.
For general pain and discomfort:
- Antispasmodics like hyoscine (Levsin) or dicyclomine (Bentyl): These relax gut muscles. About 55% of people get relief from cramping and pain.
- Low-dose antidepressants like amitriptyline (10-30 mg at night): Not for depression. These help by calming the nerves between your gut and brain. Studies show 40-50% of people feel better overall after a few weeks.
Don’t expect instant results. Antidepressants can take 4-8 weeks to kick in. Linaclotide might cause diarrhea at first. It’s trial and error. What works for your friend might not work for you.
What Else Can Help Beyond Pills?
Medication isn’t the only path. Many people find lasting relief with lifestyle changes.The low-FODMAP diet is the most researched dietary approach. Done right-with a dietitian-it helps 50-75% of people. It’s not about cutting out forever. It’s a three-step process: eliminate high-FODMAP foods for 2-6 weeks, then slowly add them back one at a time to find your triggers. Most people discover they can eat some of these foods again, just not in large amounts.
Therapy can be just as powerful as pills. Gut-directed hypnotherapy and cognitive behavioral therapy (CBT) have been shown to reduce symptoms as effectively as medication. These help retrain your brain’s response to gut signals. In one study, 60% of patients saw major improvement after 12 sessions.
Probiotics are tricky. Not all of them help. Only a few strains, like Bifidobacterium infantis 35624, have strong evidence. Most store-bought probiotics? They’re a waste of money. Stick to ones backed by research.
Stress management matters. Yoga, breathing exercises, walking, or even journaling can lower your overall symptom load. Your gut doesn’t care if your boss is annoying-it just reacts. Reducing stress doesn’t cure IBS, but it gives you back control.

What’s on the Horizon?
Science is moving fast. Researchers are looking at the gut microbiome like a fingerprint-each IBS subtype has its own bacterial signature. Fecal microbiota transplants (FMT), where healthy donor stool is given to restore gut balance, are showing promise. In one trial, 35% of IBS patients went into remission after FMT, compared to just 15% in the placebo group.New drugs like ibodutant, which targets nerve receptors in the gut, are in phase 2 trials and showing 45% symptom improvement. The FDA gave it breakthrough status, meaning it could be approved faster if results hold up.
But here’s the truth: no matter how many new drugs come out, personalized care will always win. There’s no app that will cure IBS. No supplement. No miracle tea. It’s about finding the right mix of diet, therapy, and medication for your body.
What to Do Next
If you think you have IBS:- Track your symptoms for a few weeks. Note what you eat, your stress levels, and your bowel movements.
- See your doctor. Don’t dismiss it as "just stress." Ask for a celiac test and blood work.
- Ask about a referral to a dietitian who knows FODMAPs.
- Consider therapy if stress is a big trigger.
- Don’t rush into expensive supplements. Stick to what’s proven.
IBS doesn’t define you. You can still travel, eat out, work, and live well. It just takes patience, the right tools, and knowing you’re not alone.
Can IBS turn into Crohn’s disease or colon cancer?
No. IBS is a functional disorder-it doesn’t cause inflammation, damage to the gut lining, or increase cancer risk. But its symptoms can mimic those of Crohn’s, colitis, or colon cancer. That’s why doctors rule out those conditions first, especially if you’re over 45, have weight loss, bleeding, or a family history of bowel disease.
Is the low-FODMAP diet permanent?
No. The low-FODMAP diet is a tool for identifying triggers, not a lifelong restriction. After 2-6 weeks of elimination, you slowly reintroduce foods to see which ones bother you. Most people end up eating a varied diet-just avoiding their personal triggers in large amounts. Cutting out all FODMAPs forever can hurt your gut bacteria long-term.
Why do I feel worse during my period?
Hormones like estrogen and progesterone affect how fast food moves through your gut. Right before and during your period, these hormone levels drop, which can slow digestion and increase sensitivity. About 60-70% of women with IBS report worse symptoms during this time. Tracking your cycle alongside your symptoms can help you prepare-maybe avoid high-FODMAP foods or extra stress during those days.
Do probiotics help with IBS?
Only specific strains. Most probiotics on shelves won’t help. The only one with strong evidence is Bifidobacterium infantis 35624, sold as Align or in clinical trials. It improved symptoms in about 35% of users-slightly better than placebo. Other strains? No consistent benefit. Don’t waste money on multi-strain blends unless your doctor recommends one backed by research.
How long does it take for IBS medication to work?
It varies. Loperamide works within hours. Rifaximin may show results in 1-2 weeks. Linaclotide and plecanatide often take 1-2 weeks, but full effects can take 4-6 weeks. Low-dose antidepressants like amitriptyline need 4-8 weeks at a steady dose before you’ll notice improvement. Patience is key. If nothing works after 8 weeks, talk to your doctor about switching or adding therapy.


i swear this whole ibs thing is just big pharma pushing pills so we keep buying them. they dont want you to know the real cause: 5g towers messing with your gut bacteria. i tried turning off my wifi for a week and my bloating vanished. no joke. also, dont trust any doctor who says its 'functional'... that's just code for 'we dont know what's wrong'.