Glaucoma Risk Assessment Tool
Medication-Induced Glaucoma Risk Calculator
Determine your risk for acute angle-closure glaucoma based on your medical profile and medications. This tool helps identify if you should consult an eye specialist before taking certain drugs.
Your risk assessment will appear here after clicking "Calculate Your Risk"
Imagine waking up with a throbbing headache, blurred vision, and halos around lights-then realizing your eye feels like it’s about to burst. This isn’t a migraine. It’s acute angle-closure glaucoma triggered by a common medication. And it can steal your sight in less than 24 hours if no one recognizes it.
What Exactly Is Medication-Induced Acute Angle-Closure Glaucoma?
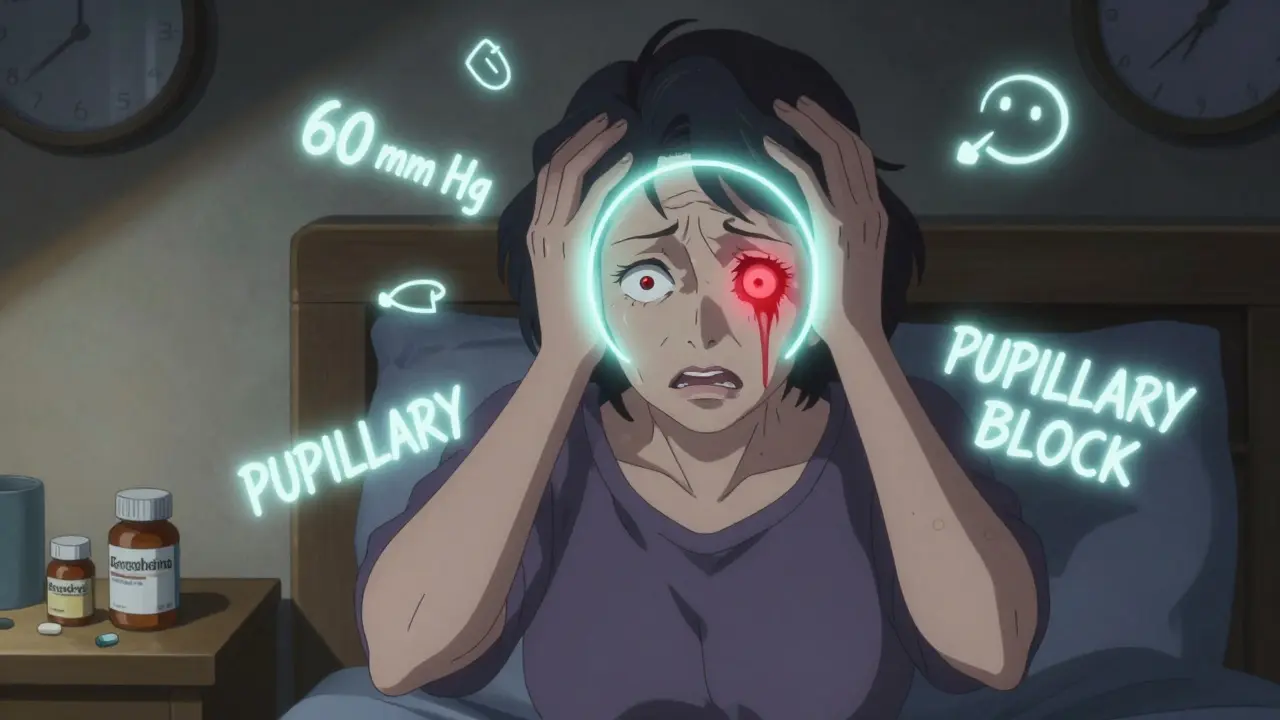
Acute angle-closure glaucoma (AACG) happens when the drainage channel in your eye suddenly gets blocked. Normally, fluid called aqueous humor flows out through a mesh-like structure called the trabecular meshwork. When that channel closes, pressure builds up fast-sometimes hitting 60 to 80 mm Hg. Normal eye pressure is under 21 mm Hg. At these levels, your optic nerve starts dying within hours.
Most people think glaucoma is slow and silent. That’s true for open-angle glaucoma. But drug-induced AACG is the opposite. It’s sudden, painful, and dangerous. And it’s not rare. About 10 to 15% of all acute glaucoma cases come from medications. In some populations, like East Asians, the risk is even higher because their eyes naturally have shallower front chambers.
How Do Medications Cause This?
It’s not the drug itself-it’s what it does to your eye’s anatomy. If you have narrow angles (which most people don’t know they have), certain drugs can push the iris forward or swell the ciliary body, blocking the drainage system. Three main ways this happens:
- Pupillary block: The pupil dilates and sticks to the lens, trapping fluid behind it and pushing the iris forward like a curtain closing off the drain.
- Plateau iris: The iris is shaped in a way that it’s already close to the drainage angle, and a drug just nudges it into place.
- Ciliary body swelling: Some drugs make the ciliary body (the muscle that controls lens shape) swell, which pushes the iris forward too.
These aren’t theoretical risks. They’re documented in real patients. A 2019 study found that over 80% of medication-induced AACG cases happen in people who had no prior symptoms or diagnosis of glaucoma. They were just taking a cold medicine or an antidepressant-and didn’t know their eyes were ticking time bombs.
Which Medications Are the Biggest Risks?
Not all drugs are equal when it comes to eye danger. Some are far more likely to trigger AACG. Here are the top offenders:
- Adrenergic agents like phenylephrine (found in nasal decongestants and some eye drops)-responsible for 35% of cases.
- Anticholinergics like tropicamide (used in eye exams) and diphenhydramine (Benadryl)-28% of cases.
- Sulfonamide-based drugs like acetazolamide and topiramate-15% of cases. These can cause fluid buildup behind the iris.
- SSRIs and tricyclic antidepressants like paroxetine and amitriptyline-12% of cases. They block acetylcholine, which keeps the pupil small and the angle open.
- Antihistamines and decongestants like pseudoephedrine-10% of cases.
Here’s the scary part: you might not even realize you’re taking one. Pseudoephedrine is in many allergy and cold medicines. Tropicamide is used routinely during eye exams. Even over-the-counter sleep aids often contain diphenhydramine.
Who’s Most at Risk?
You don’t need to have glaucoma to be at risk. You just need to have narrow angles. And most people don’t know they do.
- People over 40
- Those with farsightedness (hypermetropia)
- People with short eyeballs (axial length under 22 mm)
- Those with shallow anterior chambers (less than 2.5 mm deep)
- East Asian, Inuit, and Indigenous populations-up to 8.5% have narrow angles, compared to 3.8% in White populations
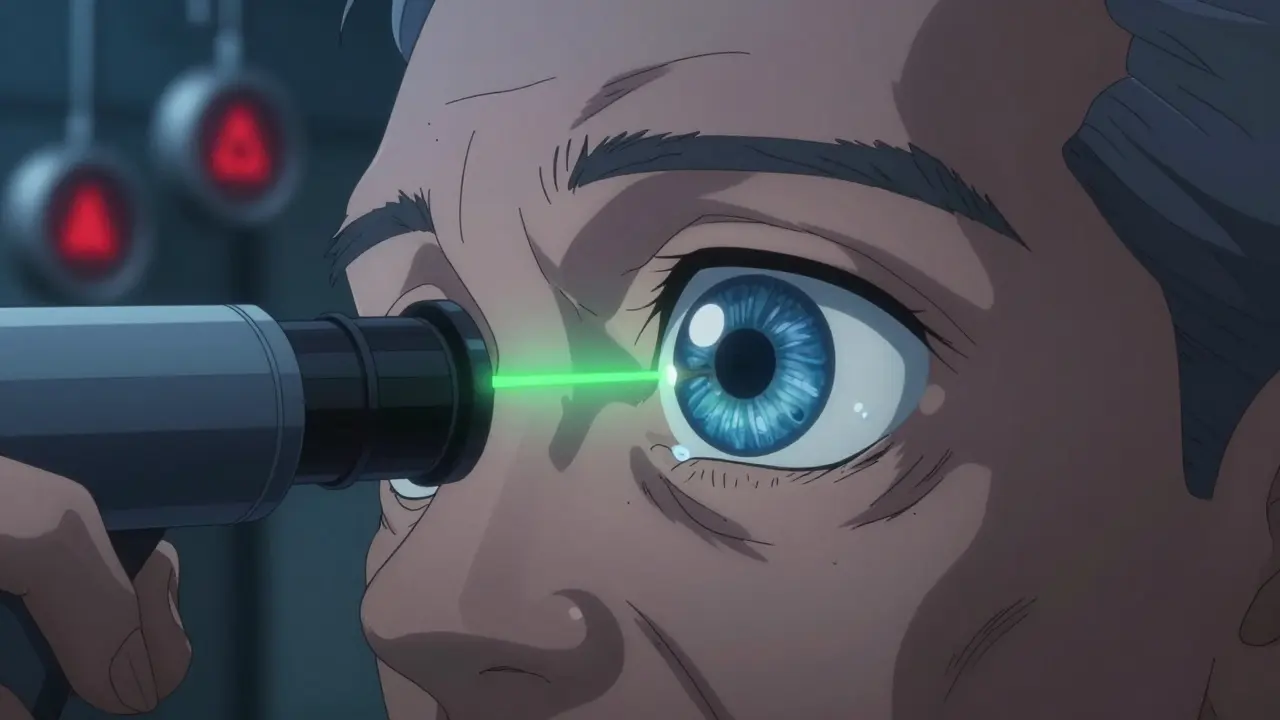
Ultrasound biomicroscopy and optical coherence tomography (OCT) can measure these traits. But unless you’ve had a gonioscopy-a quick, painless exam where a special lens is placed on the eye to view the drainage angle-there’s no way to know. And most primary care doctors don’t do it before prescribing high-risk meds.
What Are the Symptoms? Don’t Wait.
If you’re taking one of these drugs and suddenly feel:
- Severe eye pain or headache
- Blurred or cloudy vision
- Halos around lights
- Nausea or vomiting
- A red eye that won’t go away
- A pupil that looks fixed and mid-dilated (4-6 mm, doesn’t react to light)
-then you’re having an emergency. This isn’t a migraine. This isn’t a sinus infection. This is your vision slipping away. Studies show that if eye pressure stays above 40 mm Hg for more than 24 hours, permanent vision loss is likely. And in 62% of cases, patients are misdiagnosed at first-often sent home with painkillers or migraine meds.
One patient on Reddit described waking up after an eye exam with “60 mm Hg pressure and permanent damage.” Another, after taking pseudoephedrine, was told it was a migraine-then lost 20% of their peripheral vision before being correctly diagnosed 36 hours later.
How Is It Treated?
Time is vision. Treatment starts immediately:
- Pilocarpine eye drops (2%)-given every 15 minutes for an hour. This shrinks the pupil and pulls the iris away from the drainage angle.
- Intravenous mannitol-a powerful osmotic agent that pulls fluid out of the eye to lower pressure fast.
- Laser peripheral iridotomy-a tiny hole is burned in the iris to create a new drainage path. This is usually done within 24 hours and prevents future attacks.
- Stopping the triggering medication-immediately and permanently.
Without this sequence, permanent damage happens. Even with treatment, some patients lose part of their vision. That’s why prevention matters more than cure.

How Can You Prevent It?
The good news? This is one of the most preventable causes of blindness.
If you’re over 40 or have any risk factors:
- Ask your eye doctor for a gonioscopy. It takes five minutes. No pain. No drops. Just a special lens on your eye.
- If your angles are narrow (Shaffer grade ≤2), avoid all anticholinergics, sulfonamides, and adrenergic stimulants.
- Ask your doctor for alternatives: use loratadine instead of diphenhydramine; use formoterol instead of epinephrine for asthma; choose non-sulfa antibiotics if possible.
- Check OTC labels. If it says “may cause blurred vision” or “avoid if you have glaucoma,” it’s a red flag.
- Keep a list of all your medications and share it with every doctor you see-even your dentist.
Some electronic health systems, like Epic, now flag high-risk prescriptions for patients with known narrow angles. But not all clinics use them. You have to be your own advocate.
Why Is This Still Happening?
In 2023, a survey by the American Academy of Ophthalmology found that only 42% of primary care doctors routinely screen for glaucoma risk before prescribing high-risk drugs. And 68% of patients say they were never warned about eye risks when given these medications.
It’s not negligence-it’s lack of awareness. Most doctors don’t think about the eye when prescribing a cold pill. But your eye is part of your body. And some drugs don’t just affect your nose or mood-they can blind you.
Regulatory agencies like the FDA now require black box warnings on drugs like topiramate and sulfonamides. But warnings on a label don’t help if no one reads them.
What’s Next?
Research is moving fast. Scientists have found 17 genetic markers linked to narrow angles. In the next few years, a simple DNA test could tell you if you’re at risk before you ever take a single pill.
For now, though, the best defense is knowledge. If you’re over 40, or have farsightedness, or are being prescribed any of the high-risk drugs listed here-ask for a simple eye exam. Ask for gonioscopy. Ask if your medication could affect your eyes.
One question could save your sight.
Can over-the-counter cold medicine cause acute angle-closure glaucoma?
Yes. Medications containing pseudoephedrine, phenylephrine, or diphenhydramine can trigger acute angle-closure glaucoma in people with narrow iridocorneal angles. These are common in cold, allergy, and sleep aids. If you have risk factors like farsightedness or are over 40, avoid these unless cleared by an eye doctor.
Is acute angle-closure glaucoma reversible?
If treated within 24 hours, vision loss can often be prevented. But if pressure stays high for more than 24-72 hours, optic nerve damage becomes permanent. The sooner treatment starts, the better the outcome. Delayed diagnosis leads to irreversible vision loss in up to 44% of cases.
Do eye drops used during eye exams cause this?
Yes. Tropicamide and other dilating drops can trigger acute angle-closure glaucoma in people with narrow angles. That’s why eye doctors should perform gonioscopy before using these drops-especially in patients over 40 or with a family history of glaucoma. Many cases of medication-induced AACG happen after routine eye exams because this screening step is skipped.
Can I be tested for narrow angles before taking high-risk meds?
Yes. A simple test called gonioscopy, performed by an optometrist or ophthalmologist, can check your drainage angle in under 10 minutes. It’s painless and doesn’t require dilation. If you’re over 40, farsighted, or of East Asian descent, ask for this test before starting any new medication, especially antidepressants, antihistamines, or decongestants.
What should I do if I think I’m having an attack?
Go to the nearest emergency room immediately. Tell them you suspect acute angle-closure glaucoma. Mention any recent medications you’ve taken. Don’t wait for an appointment. Don’t assume it’s a migraine. Time is critical-every hour without treatment increases the risk of permanent blindness.

I can't believe we're still letting Big Pharma get away with this. My mom went blind in one eye after taking Benadryl for allergies. They told her it was 'just a migraine.' 😤 I'm filing a lawsuit and I'm not alone. #WakeUpAmerica