Many older adults are switching from brand-name drugs to generics to save money - and for good reason. Generic medications cost, on average, 80% less than their brand-name equivalents. For seniors on fixed incomes, that’s not just a convenience; it’s a lifeline. But here’s the problem: nearly half of elderly patients don’t believe generics work as well or are as safe as the originals. And while science says they’re the same, real-world experience tells a more complicated story.
Why Do Elderly Patients Doubt Generics?
It’s not just fear. It’s familiarity. Many seniors have taken the same pill for 15 years - the same color, shape, and markings. When their pharmacist hands them a different-looking pill - maybe smaller, white instead of blue, or with a different logo - they assume something’s wrong. A 2023 study of Medicare patients in New York found that fewer than 50% believed generics were as effective as brand-name drugs. That’s not ignorance. It’s a reaction to change. The issue gets worse with health literacy. About 36% of adults over 65 struggle to read and understand basic medical instructions. When a patient sees a new pill, they might not know if it’s the same drug, a different dose, or even a completely different medicine. That confusion leads to skipped doses, double dosing, or stopping the medication altogether. And then there’s the perception gap. On Reddit’s r/geriatrics, dozens of seniors reported that after switching from Synthroid (brand) to generic levothyroxine, their fatigue, weight gain, and brain fog returned. While clinical studies haven’t proven a consistent difference in effectiveness, those personal stories matter. For someone managing a chronic condition, even a small change can feel like a loss of control.Are Generics Really the Same?
Yes - and here’s why. The FDA requires generics to contain the exact same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove bioequivalence: meaning the body absorbs the drug at the same rate and to the same extent, within a narrow 80-125% range. That’s not a loophole. That’s a strict standard. For most drugs - like blood pressure pills, statins, or diabetes medications - this works perfectly. Medicare data shows 82% of seniors report no difference when switching to generics for hypertension. The average annual savings? Around $327 per person. That’s money that can go toward groceries, heating, or a needed dental visit. But not all drugs are created equal. Some have what’s called a narrow therapeutic index - meaning the difference between a helpful dose and a harmful one is tiny. Warfarin (a blood thinner) is the classic example. Even a small variation in absorption can lead to dangerous clots or bleeding. A 2021 Canadian study of over 134,000 patients found a 18.3% higher risk of emergency room visits within 30 days after switching warfarin formulations. That’s why the American Geriatrics Society recommends no automatic substitution for warfarin without close monitoring of INR levels. Other high-risk drugs include thyroid medications (like levothyroxine), seizure drugs (like phenytoin), and some heart medications. For these, switching isn’t just about cost - it’s about precision. Doctors and pharmacists need to be extra careful.How Aging Changes the Way Drugs Work
As we age, our bodies don’t process medicine the same way. Kidney function drops - by age 85, nearly half of people have a creatinine clearance below 50 mL/min. The liver slows down. Body fat increases while muscle mass declines. All of this affects how drugs are absorbed, distributed, and cleared from the body. That’s why even tiny differences between brand and generic formulations can matter more in older adults. A pill that’s absorbed 5% slower might be fine for a 30-year-old. But for an 80-year-old with reduced kidney function? That 5% could push the drug level into a dangerous range. And then there’s polypharmacy. Nearly half of Medicare beneficiaries take five or more medications daily. That’s not just a lot of pills - it’s a minefield. Each additional drug increases the chance of bad interactions, side effects, or confusion. The American Geriatrics Society’s Beers Criteria lists dozens of medications that should be avoided or used with extreme caution in seniors. When you’re already on eight pills, switching one to a generic might seem harmless - but it can trigger a chain reaction.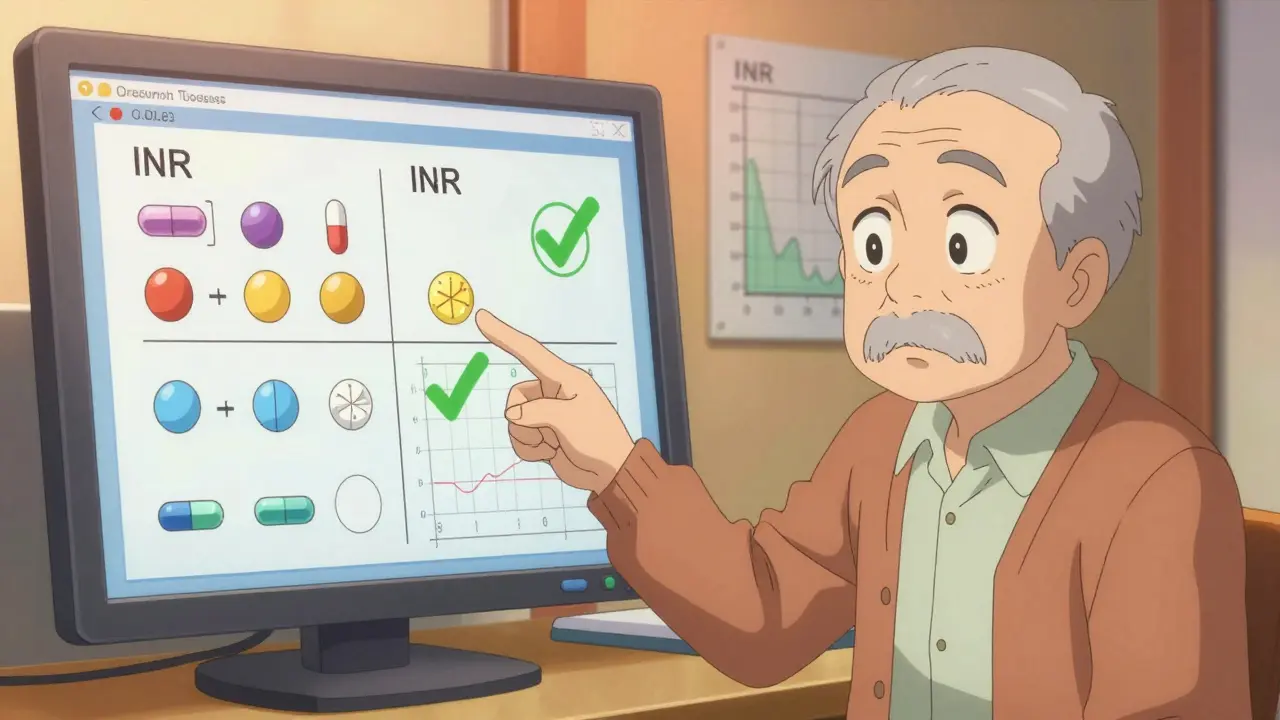
When Switching Can Be Dangerous
The biggest risks aren’t always from the drug itself - they’re from how the switch is handled. First, automatic substitution without patient knowledge. Some pharmacies automatically swap generics without telling the doctor or patient. That’s legal - but it’s not safe for seniors. Without consent or explanation, patients assume nothing changed. When symptoms return, they blame their condition, not the medication. Second, switching multiple drugs at once. A patient might get a new prescription for a generic blood pressure pill, a different generic for cholesterol, and a new generic for pain - all in the same visit. If they start feeling dizzy or confused, they can’t tell which one caused it. That’s why experts recommend switching one drug at a time - and waiting at least two to four weeks before changing another. Third, OTC confusion. Many seniors take over-the-counter painkillers like ibuprofen or acetaminophen daily. But generic versions often come in multi-symptom formulas - like “Advil Cold & Sinus” or “Tylenol PM.” These contain hidden ingredients that can interact with prescription meds or cause liver damage. A 2017 NIH study found that 45% of acetaminophen use among seniors was dangerous because of hidden doses in combination products.How to Switch Safely
Switching to generics isn’t something to do on a whim. It needs a plan.- Ask your doctor before any switch. Not all generics are equal - especially for narrow therapeutic index drugs.
- Get the same generic each time. If your pharmacy switches suppliers, the pill might look different again. Ask to stick with one brand of generic.
- Use the teach-back method. After your pharmacist explains the switch, ask them to show you the pill and say: “Tell me in your own words why this is the same as my old one.” This simple step improves adherence by 42%.
- Keep a medication list - written down, not just in your head. Include the name, dose, purpose, and whether it’s brand or generic. Bring it to every appointment.
- Watch for changes. If you feel different - more tired, dizzy, confused, or if your symptoms return - call your doctor. Don’t wait. Don’t assume it’s “just aging.”

What Works Best for Seniors
The most successful programs don’t just push generics - they support patients through the change. A 2024 JAMA study showed that when clinical pharmacists joined care teams for elderly patients, they reduced inappropriate medications by 37%. These pharmacists didn’t just check pills - they sat down with patients, showed them side-by-side images of brand vs. generic pills, explained why they were the same, and checked in after the switch. Computerized systems that alert doctors when a senior is on too many drugs or a risky combination also help. One hospital system cut ADE-related ER visits by 29% just by adding these alerts to electronic records. And the best tool? Simple visuals. A photo of the old pill next to the new one. A label that says, “This is the same medicine, just cheaper.” A calendar that tracks when the switch happened. These aren’t fancy tech - they’re common sense.The Big Picture: Cost vs. Care
The U.S. spent $61.7 billion on generic drugs in 2023 - saving Medicare beneficiaries an average of $602 per person annually. That’s billions in savings. But savings mean nothing if patients stop taking their meds because they’re scared or confused. The goal isn’t just to switch more people to generics. It’s to switch them safely. That means time - time for counseling, time for monitoring, time for trust. By 2030, nearly 94% of Medicare prescriptions will be generic. That’s progress. But without better communication, better education, and better support, we’ll still see avoidable hospital visits, falls, and worsening conditions - not because generics don’t work, but because we didn’t help people understand how to use them.What’s Next?
The American Geriatrics Society is updating its guidelines for emergency departments in late 2024 - and for the first time, they’re requiring pharmacists to be part of the care team for seniors on multiple drugs. Three NIH-funded studies are now tracking seniors aged 75+ who’ve switched to generics, looking at long-term outcomes like falls, hospital stays, and cognitive decline. Meanwhile, the government is cracking down on dangerous OTC combinations. New labeling rules will require clearer warnings on multi-symptom pain relievers. The science is clear: generics are safe and effective for most seniors. But the human side? That’s still a work in progress. And that’s where the real challenge lies.Are generic medications really as effective as brand-name drugs for elderly patients?
Yes, for most medications. The FDA requires generics to contain the same active ingredient, strength, and dosage form as the brand-name version, and they must prove they’re absorbed by the body at the same rate and level. For common drugs like blood pressure pills, statins, or diabetes medications, studies show no difference in effectiveness for seniors. However, for drugs with a narrow therapeutic index - like warfarin or levothyroxine - even small differences can matter. These require careful monitoring after a switch.
Why do some elderly patients feel worse after switching to generics?
Many report feeling different because the pill looks different - smaller, different color, or different markings. This can trigger anxiety or the belief that the medicine isn’t working. In rare cases, especially with drugs like levothyroxine or warfarin, minor differences in absorption can affect how the body responds. But these aren’t always due to the generic itself - they can also come from switching multiple drugs at once, missing doses, or interactions with other medications. Always report changes to your doctor.
Which medications should not be switched to generics in elderly patients?
The American Geriatrics Society advises caution with drugs that have a narrow therapeutic index - where the difference between a safe and dangerous dose is small. These include warfarin (blood thinner), levothyroxine (thyroid hormone), phenytoin (seizure control), and some anti-seizure and heart rhythm medications. Automatic substitution without close monitoring is not recommended. Always discuss switching these with your doctor before making any changes.
Can switching to generics cause dangerous drug interactions?
Switching itself doesn’t cause interactions - but doing it carelessly can. The real danger comes when multiple drugs are switched at once, or when patients start taking over-the-counter meds like ibuprofen or acetaminophen without realizing they’re already in their prescription pills. For example, many seniors take Tylenol PM, which contains diphenhydramine - a sedative that can worsen confusion and increase fall risk. Always review all medications - prescription and OTC - with your pharmacist.
How can I make sure I’m taking my generic medication correctly?
Ask your pharmacist to show you the pill and explain why it’s the same as your old one. Use the teach-back method: repeat back what they told you in your own words. Keep a written list of all your medications, including whether they’re brand or generic. Take them at the same time every day. Don’t switch more than one drug at a time. If you feel different - tired, dizzy, confused - call your doctor right away. Don’t wait.
Is it safe to let my pharmacy switch my medication without telling me?
Legally, yes - but it’s not always safe. Pharmacists can automatically substitute generics unless your doctor writes “dispense as written” on the prescription. But for seniors, especially those on multiple medications or with memory issues, this can lead to confusion, missed doses, or side effects. Always ask to be notified before any switch. You have the right to know what you’re taking and why.
What should I do if I think my generic medication isn’t working?
Don’t stop taking it. Call your doctor or pharmacist. Write down what changed - when you switched, what symptoms returned, and how you’re feeling. Bring your medication list. Your doctor may check your blood levels (like INR for warfarin or TSH for thyroid meds) or suggest switching back temporarily to see if symptoms improve. Never assume it’s just aging - it could be the medication.


Generics are the unsung heroes of geriatric care. I’ve seen grandmas on fixed incomes breathe easier because they can actually afford their meds. The science is rock solid - bioequivalence isn’t a suggestion, it’s a federal mandate. Sure, some folks feel weird when the pill changes color, but that’s psychology, not pharmacology. We need more education, not fear-mongering.