When you walk up to the pharmacy counter to pick up your prescription, you might think the hardest part is waiting in line. But for pharmacists, that moment is one of the most critical safety checks in healthcare. Confirming allergies and interactions at pickup isn’t just a formality-it’s the last line of defense against a potentially life-threatening mistake. Every year, tens of thousands of people end up in the hospital because a medication clashed with something they were already taking-or something their body can’t handle. And most of those errors happen right at the point of dispensing.
Why This Step Can’t Be Skipped
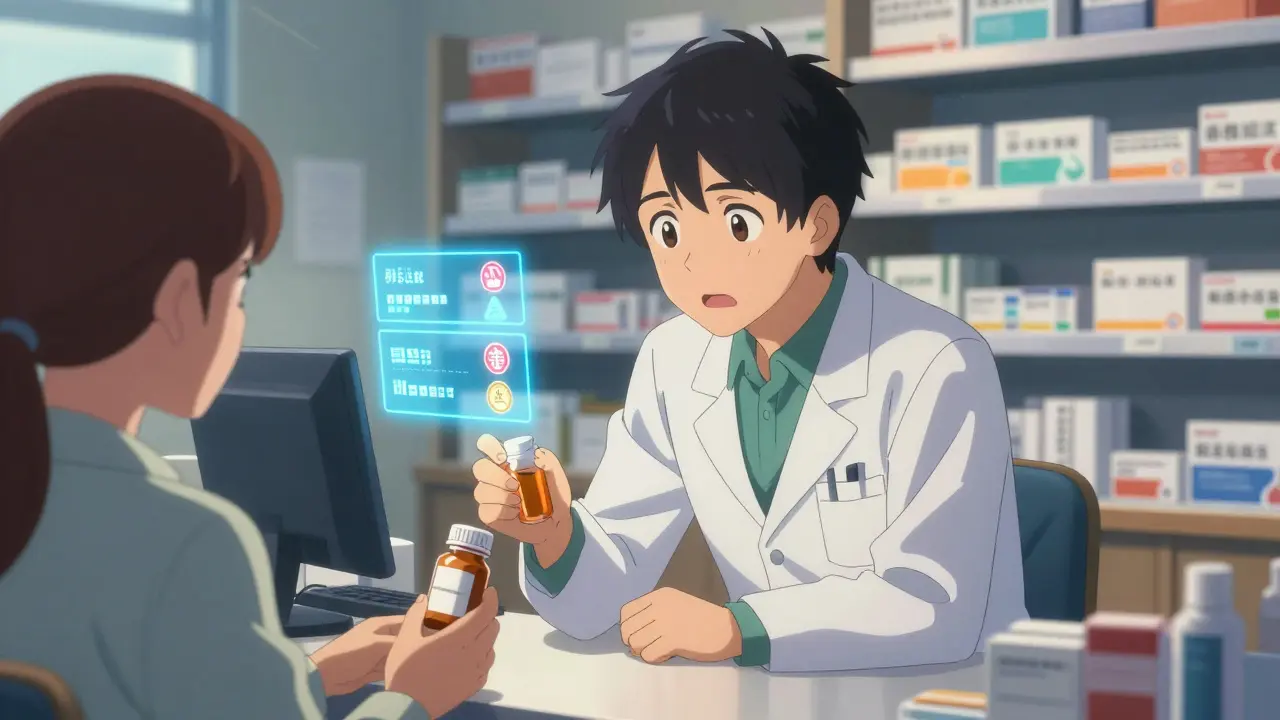
You’ve probably seen the sticker on your prescription bottle: "Allergy to penicillin?" Or maybe you’ve been asked, "Are you allergic to any meds?" again-even though you’ve said it three times before. It’s frustrating. But here’s the truth: 90% of patients who say they’re allergic to penicillin aren’t actually allergic. That’s not a typo. Studies show most people outgrow it, or were misdiagnosed as kids after a rash that had nothing to do with an immune reaction. Yet the label sticks in the system, and pharmacies are forced to treat it as real. That’s why pharmacists don’t just rely on what’s in the computer. They cross-check three things: your documented allergies, your current meds, and the new prescription. If you’re on blood pressure medicine and the pharmacist sees you’re being given a new NSAID like ibuprofen, they’ll flag it. Why? Because together, they can spike your blood pressure or damage your kidneys. That’s not theoretical. In 2022, the Journal of the American Medical Informatics Association analyzed 4.7 million prescriptions and found that properly configured systems catch 99.8% of real interactions.How the System Works Behind the Counter
The process starts the moment the prescription hits the pharmacy system. Most pharmacies use software tied to your electronic health record (EHR). These systems pull your allergy list from your doctor’s notes and compare it against every ingredient in the new drug-not just the active one, but the fillers too. That’s why you might get an alert for "dye allergy" when you’ve never mentioned it. The system doesn’t know if you’re allergic to Red 40 or just think you are. It’s programmed to err on the side of caution. There are two main ways these systems screen:- Drug name concept screening: Checks the active ingredient (like amoxicillin) against all known interactions. This catches 3.2 times more real risks than older methods.
- NDC-based screening: Uses National Drug Codes to match exact pill formulations. It’s precise but outdated-NDC codes expire when drugs get reformulated, leading to missed alerts.
What Pharmacists Actually Do at Pickup
You might think they just scan the barcode and hand you the bottle. But the American Society of Health-System Pharmacists (ASHP) requires them to complete four steps in under 90 seconds:- Check if your allergy record is current-if it’s older than 12 months, they’ll ask you to confirm it.
- Run an interaction check using trusted databases like Lexicomp or Micromedex.
- Verify inactive ingredients if you have a known sensitivity (like lactose, gluten, or specific dyes).
- Document the check with a timestamp and their initials in the system.
What You Can Do to Help
You’re not just a patient. You’re part of the safety team. Here’s how you can make this process faster and safer:- Keep your allergy list updated. If you think you’re allergic to sulfa but never had a reaction, ask your doctor to test you. Many people carry false labels for decades.
- Bring a current med list. Not just prescriptions-supplements, OTC painkillers, even herbal teas. St. John’s Wort can interfere with birth control and antidepressants. No one thinks to mention it.
- Speak up if something feels off. If you’ve had a reaction to a drug before, even if it was years ago, say it. Don’t assume the system knows.
- Ask questions. If the pharmacist says, "We’re holding this because of an interaction," ask: "What’s the risk? Is there another option?" Most pharmacists are trained to explain this in plain language.
Common Pitfalls and How to Avoid Them
Even with the best systems, things go wrong. Here are the top three problems-and how to fix them:- Outdated allergy records. A 2023 University of Michigan study found over a third of allergy entries in EHRs are older than five years. If your record says "allergic to aspirin" from 2018, but you’ve taken it without issue since, tell your pharmacist. They can flag it for review.
- False positives from inactive ingredients. If you’re told you can’t take a drug because it contains "dye," ask: "Which dye?" Many patients are only allergic to specific dyes, not all. Some pharmacies now let you create a custom picklist-like "avoid Red 40, but Blue 1 is fine."
- Missing drug-condition interactions. For example, if you have kidney disease and get a new NSAID, the system might not catch it unless your condition is clearly documented. Always tell your pharmacist if you have chronic conditions like diabetes, heart failure, or liver disease.
The Bigger Picture: Why This Matters Beyond Your Prescription
This isn’t just about your next pill. Medication errors cost the U.S. healthcare system over $21 billion a year. The FDA and CMS are cracking down. By October 2024, pharmacies with more than a 15% override rate for allergy alerts will face financial penalties. That’s pushing hospitals and chains to upgrade their systems. Epic’s new release now suppresses low-severity alerts for patients with multiple allergies-so the important ones stand out. Meanwhile, AI tools are starting to scan clinical notes for hidden allergy clues. Google Health’s pilot program found 31.7% more undocumented allergies by reading doctor’s handwritten notes. That’s huge. It means your allergy might be hiding in plain sight.What’s Next for Medication Safety
By 2025, the FDA will require all drug labels to use standardized allergy codes (SPL format). That means your pharmacy system will know exactly what "penicillin allergy" means-whether it’s a mild rash or anaphylaxis. That’s a game-changer. In the meantime, the best tool you have is your voice. Don’t assume your pharmacist knows everything. Don’t assume your doctor updated your record. And don’t assume you’re safe just because you’ve taken the drug before. Medication safety isn’t a system. It’s a team. And you’re on it.What if I think my allergy is wrong?
If you believe your allergy label is incorrect-like being told you’re allergic to penicillin but have taken it safely before-ask your pharmacist to help you get tested. Skin tests for beta-lactam antibiotics are reliable and can clear you for 93% of mislabeled cases. Many allergists offer this as a quick, low-cost appointment. Once confirmed, ask your doctor to update your EHR and give you a note to give to your pharmacy.
Why does the pharmacist ask the same question every time?
Because your allergy status can change. You might have outgrown an allergy, developed a new one, or started a new medication that changes your risk. Pharmacists are required to verify each time as part of the ASHP 2023 protocol. It’s not about distrust-it’s about accuracy. Even a small change in your health can turn a safe drug into a dangerous one.
Can I trust the computer system completely?
No system is perfect. While modern EHRs catch 99.8% of real interactions, they still generate false alerts-especially around inactive ingredients. That’s why pharmacists are trained to review every alert. If the system flags something you know is safe, tell them. Your input helps improve the system. The best safety net is a pharmacist who listens to you.
What if I don’t remember all my medications?
Bring your pill bottles or take a photo of your medicine cabinet before your appointment. Even over-the-counter drugs like ibuprofen, antacids, or sleep aids can interact. Supplements like fish oil, garlic, or ginkgo can thin your blood and interfere with surgery or blood pressure meds. Don’t worry about being perfect-just be honest. Your pharmacist has seen it all and won’t judge.
Are there alternatives if I have an allergy or interaction?
Yes, almost always. Pharmacists are trained to find safe alternatives. For example, if you’re allergic to penicillin, there are over 15 other antibiotics that work just as well for common infections. If you can’t take NSAIDs due to kidney issues, acetaminophen or physical therapy might be options. Always ask: "Is there another choice?" It’s your right-and your pharmacist’s job to help you find it.

My pharmacist once held my script for 20 minutes because I said I was allergic to penicillin. Turned out I wasn’t. Now I just say 'nope' and walk out. Why do they even ask if they don’t listen?