Parkinson's disease: Symptoms, Treatment, and Practical Tips
Parkinson's disease is a progressive brain disorder that affects movement. Early signs are often subtle: a slight tremor, a stiff arm, changes in handwriting, or slowness when you stand up. Knowing common symptoms helps you get care earlier—treatment works best when started sooner.
Most people with Parkinson's notice motor symptoms: resting tremor, bradykinesia, rigidity, and balance problems. Non-motor signs like sleep changes, reduced sense of smell, constipation, depression, and anxiety can appear years before movement problems. If you notice a mix of these, see your doctor.
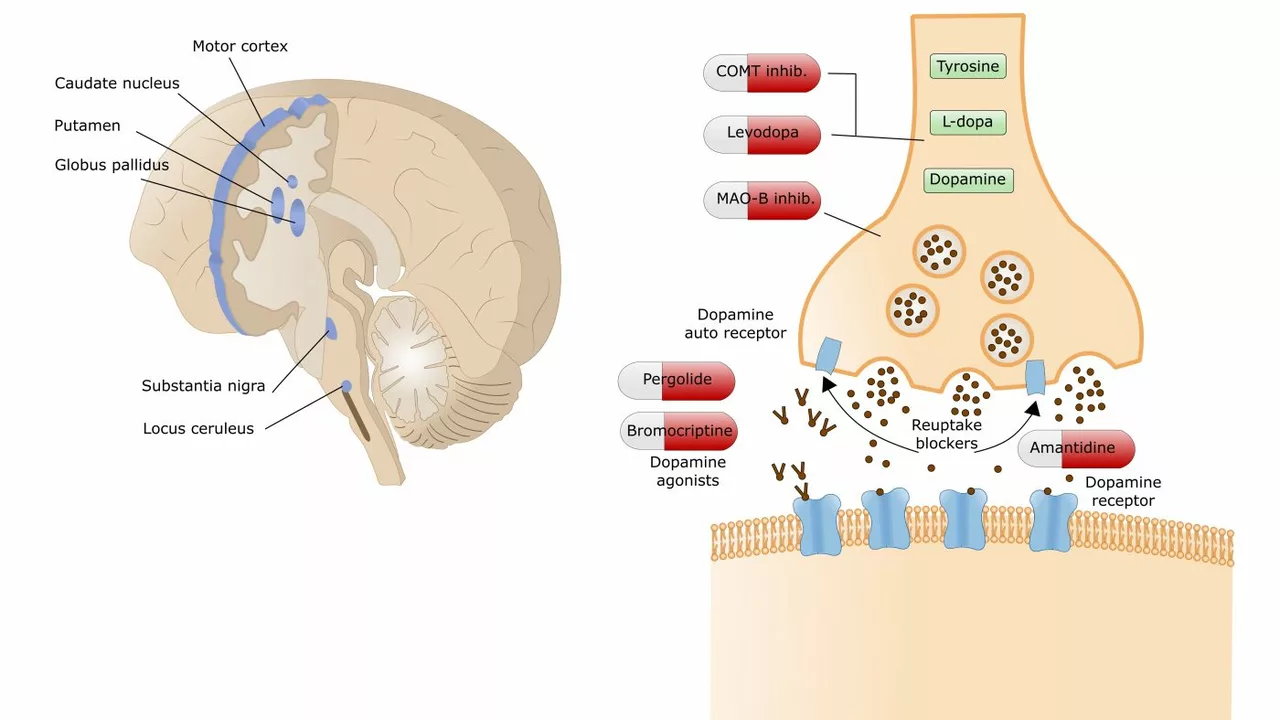
Diagnosis is clinical; neurologists use exams and medical history. Imaging like a dopamine transporter (DaT) scan can support a diagnosis but does not replace clinical judgment. Getting a second opinion from a movement-disorder specialist is worth it if symptoms are unclear or progress differently than expected.
Treatment options that help day to day
Levodopa is the most effective medication for motor symptoms. It converts into dopamine and usually improves walking, tremor, and stiffness. Other drugs—dopamine agonists, MAO-B inhibitors, and COMT inhibitors—are added to smooth symptoms or delay levodopa side effects. Each drug class has pros and cons; discuss side effects like sleepiness, impulsive behavior, or blood pressure drops with your doctor.
Physical therapy, occupational therapy, and speech therapy make a big difference in daily life. PT focuses on walking, balance, and strength. OT teaches safer ways to do dressing, cooking, and personal care. Speech therapy helps with swallowing and voice problems. Regular, goal-focused exercise is one of the strongest things you can do to stay mobile.
Managing complications and staying independent
Motor fluctuations and dyskinesias can develop after years of levodopa use. Keep a symptom and medication diary—note “on” times when meds work well and “off” times when they don’t. This helps your team adjust doses or consider options like controlled-release formulations, apomorphine pumps, or deep brain stimulation (DBS) for eligible patients.
Sleep, mood, and cognition deserve attention. Insomnia, vivid dreams, depression, anxiety, and mild cognitive changes are common. Treating sleep and mood improves quality of life for both patients and caregivers. Non-drug strategies—sleep routines, light exposure, therapy—help alongside medications when needed.
Practical home changes reduce fall risk: clear walkways, remove loose rugs, add grab bars, improve lighting, and use chairs with firm armrests. Adaptive devices—reacher tools, button hooks, weighted utensils—can preserve independence. A home safety review by an occupational therapist is worth it.
Nutrition and hydration matter. Constipation is common; fiber, fluids, and movement help. Some protein can interfere with levodopa absorption—spacing protein intake evenly through the day or timing protein away from medication can help, but discuss changes with your clinician.
Clinical trials and new therapies are active areas of research, from gene therapies to focused ultrasound and new drug classes. If you’re interested, ask your neurologist about trials suitable for your stage. Joining a support group helps you learn from others and access local resources.
Parkinson’s care is a team effort. Work with neurologists, therapists, nurses, pharmacists, and social workers to build a plan around your goals. Early diagnosis, regular exercise, medication management, and practical changes at home keep people living well.
The Role of Calcitriol in Parkinson's Disease and Neurodegeneration
In my latest research, I've been exploring the role of Calcitriol in Parkinson's Disease and neurodegeneration. Calcitriol, the active form of Vitamin D, has been found to have neuroprotective effects, potentially slowing the progression of diseases like Parkinson's. Some studies suggest it could reduce inflammation and oxidative stress in the brain, which are linked to neurodegeneration. However, more research is needed to fully understand its impact. While it's not a cure, it's a promising avenue that could lead to better management of neurodegenerative conditions.
More Detail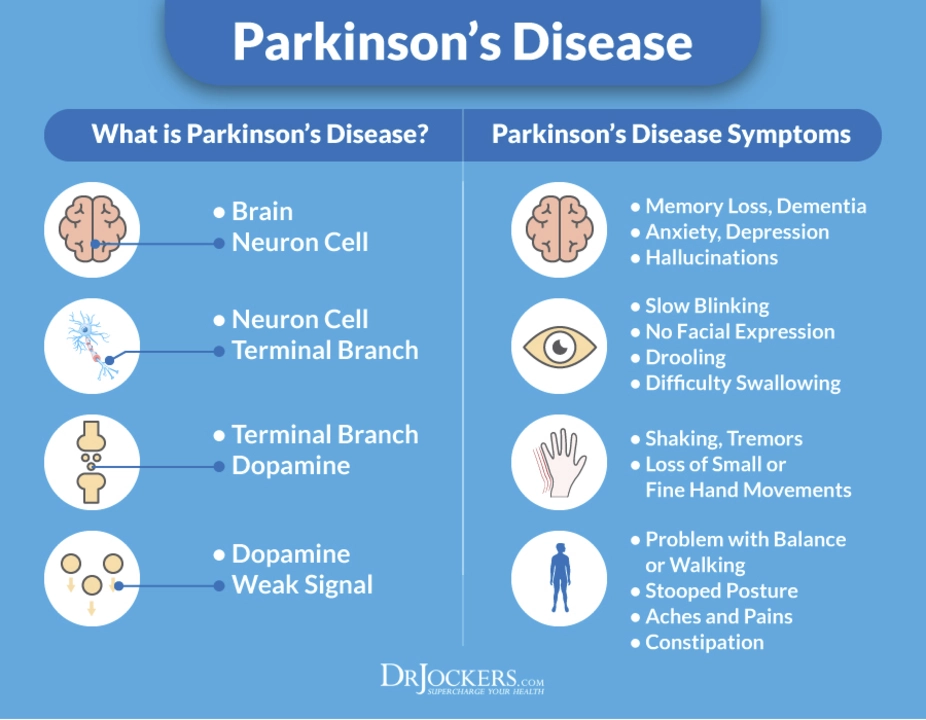
The Role of Trihexyphenidyl in Occupational Therapy for Parkinson's Disease
As a blogger, I've recently come across the topic of Trihexyphenidyl and its role in occupational therapy for Parkinson's Disease. Trihexyphenidyl is an anticholinergic medication that helps alleviate symptoms like tremors and muscle stiffness in Parkinson's patients. In occupational therapy, this medication can significantly improve a patient's ability to perform daily tasks and maintain their independence. It is essential to note that while Trihexyphenidyl is beneficial, it may not work for everyone, and it's crucial to work closely with healthcare professionals to find the best treatment plan. Overall, Trihexyphenidyl has shown promising results in helping Parkinson's patients lead more fulfilling and independent lives through occupational therapy.
More Detail