Acetaminophen Safety Calculator
Add Medications
Current Intake
Safety Recommendations
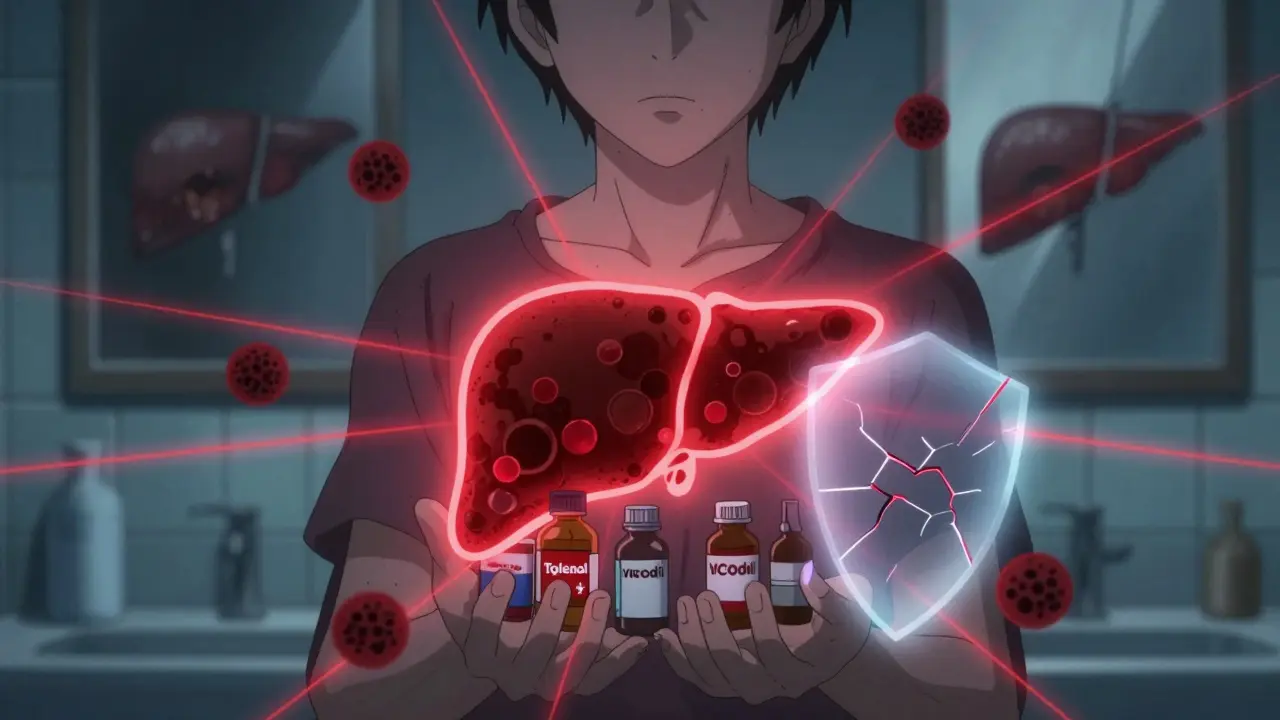
Every year, thousands of people end up in the hospital not because of a bad fall or a bad infection, but because they took something they thought was harmless: acetaminophen. It’s in Tylenol, in cold medicines, in painkillers like Vicodin and Percocet, and even in some sleep aids. For most people, it’s safe. But if you have liver disease - or even if you just drink alcohol regularly - that same pill can turn into a silent killer.
Why Acetaminophen Is Dangerous for Your Liver
Acetaminophen works great for fever and pain. Your body breaks it down mostly through two safe pathways: sulfation and glucuronidation. But when you take too much - even just a little too much over time - those pathways get overwhelmed. Then your liver starts using a backup system: cytochrome P450. This system produces a toxic byproduct called NAPQI. Normally, your liver neutralizes it with glutathione, an antioxidant. But if you’ve already used up your glutathione - from drinking alcohol, being malnourished, or having liver damage - NAPQI starts eating away at your liver cells.
This isn’t theoretical. In the U.S., acetaminophen overdose causes about 1,600 cases of acute liver failure each year. Around 500 people die. That’s more than any other single drug. And most of these cases aren’t suicide attempts. They’re mistakes.
The Numbers That Can Kill You
Most people think the limit is 4,000 mg per day. That’s what’s printed on Tylenol bottles. But here’s the catch: that number is for healthy adults with no liver problems. If you have hepatitis, fatty liver disease, or cirrhosis, your liver can’t handle that much. Experts now say you should cut that limit in half - no more than 2,000 mg a day.
And if you drink alcohol? Even one drink a day can make your liver more vulnerable. Some doctors say the safe daily limit for drinkers is just 2,000 mg. Others say 1,500 mg. The truth? There’s no safe number if you drink regularly. Avoid alcohol completely while taking acetaminophen.
Also, don’t assume that extra-strength Tylenol is the same as regular. Extra-strength pills are 500 mg each. Two pills four times a day = 4,000 mg. Now add a cold medicine with acetaminophen - say, NyQuil - and you’ve hit 5,000 mg. That’s over the limit. And you didn’t even mean to.
Mayo Clinic says some products, like Tylenol Extra Strength, now recommend a max of 3,000 mg per day. That’s because they’ve seen too many people go over the limit without realizing it.
Hidden Acetaminophen Is the Biggest Risk
Here’s the real problem: acetaminophen is hiding in plain sight. It’s listed as APAP on prescription labels. It’s in combination pills with codeine, oxycodone, hydrocodone. It’s in cold and flu remedies like DayQuil, TheraFlu, and Alka-Seltzer Plus. You take one for your headache. Then you take one for your stuffy nose. Then you take one for your fever. Three different pills. All with acetaminophen. And you think you’re being careful.
That’s why poison control centers in the U.S. get more calls about acetaminophen than any other substance. People don’t know what they’re taking. They don’t read labels. Or they assume, “It’s just a cold medicine - it can’t hurt.”
One study found 21 cases where people took acetaminophen exactly as directed - no overdose - and still developed liver damage. Why? Because they were taking multiple products with the same ingredient. No one told them to add it up.

What If You Already Have Liver Disease?
If you have hepatitis B or C, non-alcoholic fatty liver disease, or cirrhosis, your liver is already working harder. It doesn’t have the backup capacity to handle extra stress. Even normal doses can push it over the edge.
Doctors now recommend that people with liver disease avoid acetaminophen entirely if possible. If you must use it, stick to 2,000 mg a day - and only for a few days at a time. Never use it for chronic pain without talking to your doctor. There are safer options: physical therapy, low-dose NSAIDs (if your kidneys are okay), or other non-drug approaches.
And if you’re on medications that boost the P450 enzyme - like some seizure drugs, tuberculosis meds, or even St. John’s Wort - your risk goes up. These drugs speed up the production of NAPQI. That means even normal doses become dangerous.
What to Do If You Think You’ve Overdosed
Acetaminophen overdose doesn’t always cause symptoms right away. You might feel fine for 24 hours. Then nausea, vomiting, and right-sided abdominal pain show up. By then, your liver might already be badly damaged.
If you suspect you’ve taken too much - even if you feel fine - go to the ER immediately. Don’t wait. Don’t call your doctor tomorrow. Go now.
The antidote is acetylcysteine (NAC). It works best if given within 8 hours of ingestion. It can still help up to 16 hours later. But after that, its effectiveness drops fast. Hospitals use the Rumack-Matthew nomogram to decide if you need it. It’s a chart that plots your blood level of acetaminophen against the time since you took it. If you’re above the treatment line, you get NAC.
Don’t worry about side effects from NAC. Some people get nauseous or have allergic reactions. But those are rarely dangerous. The risk of liver failure is far worse. If you’ve taken more than 10 grams, or more than 200 mg per kg of body weight, they’ll start NAC even before they get your blood test results. Waiting could cost you your liver.

How to Stay Safe
Here’s what you actually need to do:
- Read every label. Look for “acetaminophen,” “APAP,” or “paracetamol.” If it’s on the list, you’re taking it.
- Add it up. If you’re taking more than one medicine, write down how much acetaminophen is in each. Total it. Don’t guess.
- Never go over 3,000 mg a day. Even if you’re healthy. Lower is safer.
- Avoid alcohol completely. No exceptions. Not one beer. Not one glass of wine.
- Use the lowest effective dose. If 325 mg works, don’t take 650 mg.
- Ask your pharmacist. When you get a new prescription, ask: “Does this contain acetaminophen?”
- For kids, use the syringe. Never use a kitchen spoon. A teaspoon isn’t the same as a medicine spoon. Dosing errors in children are common and deadly.
What About Pregnant Women?
Acetaminophen is still the safest painkiller during pregnancy - but only if used correctly. The same rules apply: don’t exceed 3,000 mg a day, avoid alcohol, and don’t take it long-term. If overdose happens, NAC is safe for both mother and baby. IV and oral forms are both approved. Don’t delay treatment because you’re afraid of the medicine. The risk of liver failure is much higher.
Bottom Line
Acetaminophen isn’t dangerous because it’s bad. It’s dangerous because it’s everywhere, and people think it’s harmless. But your liver doesn’t care if you meant to take it. It only knows how much you took and whether you’ve been drinking. If you have liver disease, your margin for error is razor-thin. One extra pill. One drink. One missed label. That’s all it takes.
Don’t wait for symptoms. Don’t assume you’re safe because you’re not taking a lot. Check your meds. Add them up. Cut your daily dose in half. And if you’re not sure - don’t take it. There are other ways to manage pain. Your liver will thank you.

They’re lying about acetaminophen. It’s not about dosage-it’s about the government letting Big Pharma poison us while they profit from liver transplants. You think this is an accident? No. It’s a slow genocide disguised as medicine. I’ve seen the files. They know. They just don’t care.
And don’t even get me started on NAC. That’s not an antidote. It’s a placebo to make you feel safe while your liver turns to mush.
They’re watching. They’re recording. They’re waiting for you to take that extra pill.