Switching from a brand-name drug to a generic version is one of the most common changes in your medication routine - and for good reason. Generics save you money, often by 80% or more, and they’re just as safe and effective for most people. But if you’ve ever wondered, “What if my body reacts differently now?” - you’re not alone. While science says generics are identical in active ingredients, some people notice subtle changes. That’s why monitoring your health after switching matters - not because generics are risky, but because your body is unique.
Why Some People Notice a Difference
The FDA requires generics to deliver the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. That’s called bioequivalence. For most drugs, that’s enough. But for medications with a narrow therapeutic index - where the difference between a helpful dose and a harmful one is very small - even tiny changes in absorption can matter. Drugs like warfarin (a blood thinner), levothyroxine (for thyroid function), and certain seizure medications like lamotrigine fall into this category. Studies show that while 90%+ of people have no issue switching, a small group - often those with chronic conditions - may feel different. It’s not because the generic is bad. It’s because your body might absorb it slightly differently due to inactive ingredients, pill coating, or manufacturing variations. A 2021 study in JAMA Internal Medicine found that patients switching from brand to generic levothyroxine had a small but measurable increase in TSH levels - enough to require a dose adjustment in some cases. The same pattern showed up with lamotrigine. These aren’t failures. They’re signals. And that’s why tracking your health after the switch is critical.What to Monitor - And How
You don’t need to become a lab technician. But for the first 30 to 90 days after switching, pay attention to these signs:- For thyroid patients (levothyroxine): Track symptoms like fatigue, weight changes, heart palpitations, or mood swings. Get a TSH blood test at 4 and 8 weeks after switching. Even a 10% shift in TSH can mean your dose needs tweaking.
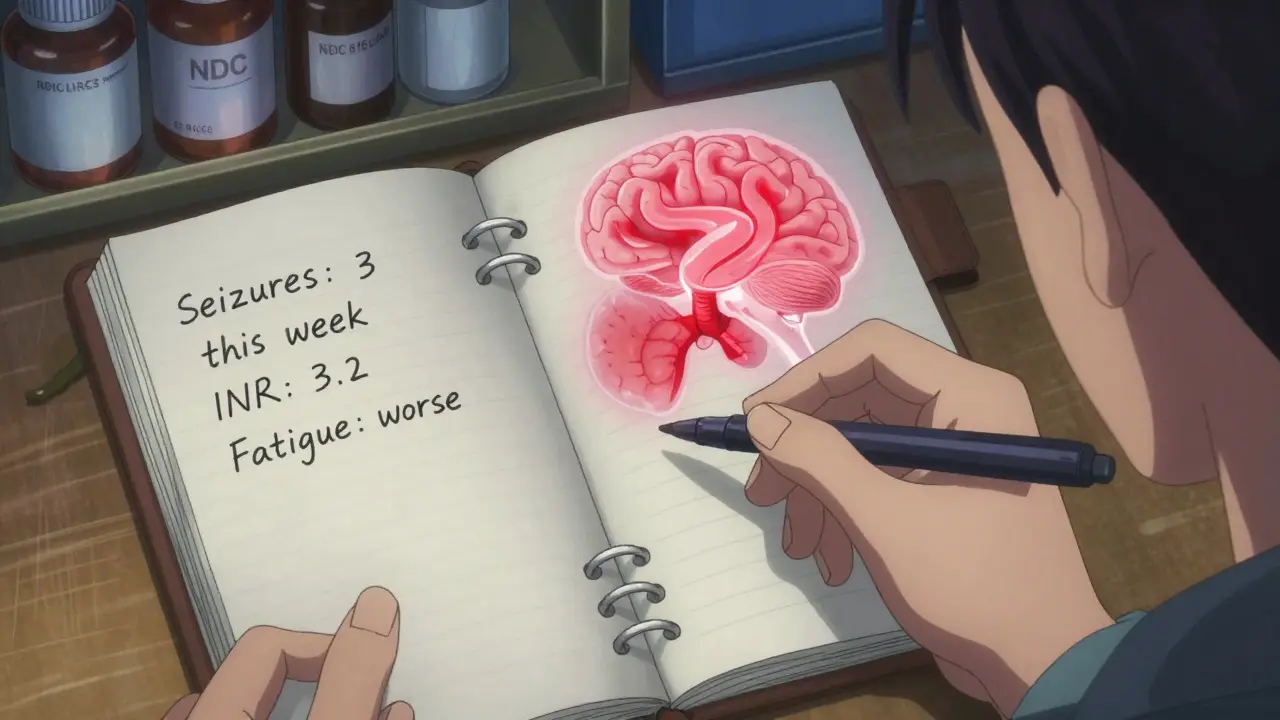
- For epilepsy or seizure disorders (lamotrigine, phenytoin): Keep a seizure diary. Note frequency, duration, and intensity. If you notice more seizures, or new types of episodes, contact your doctor immediately. The Institute for Safe Medication Practices found 62% of reported generic issues involved antiepileptic drugs.
- For blood thinners (warfarin): Monitor your INR levels more frequently - ideally every 7 to 14 days after switching. A change of 0.5 or more in INR can increase your risk of clotting or bleeding.
- For depression or anxiety (bupropion, SSRIs): Watch for changes in mood, sleep, or appetite. Some patients report feeling “off” after switching to generic bupropion, even though the active ingredient is the same. It may be due to different fillers or release mechanisms.
- For high blood pressure or diabetes: Check your blood pressure daily for two weeks. For diabetes, track fasting glucose and HbA1c at 4 and 8 weeks. If your numbers start drifting, don’t assume it’s your diet - it could be the medication.
Keep a simple log. Write down the date, your symptoms, any new side effects, and key numbers. This isn’t just for you - it’s for your doctor. When you say, “I feel different,” they need data to act on.
How to Confirm You Got the Right Generic
Not all generics are made the same. Different manufacturers use different inactive ingredients - things like dyes, fillers, or coatings. These don’t affect the drug’s action, but they can change how it dissolves in your stomach. Always check the pill’s appearance. If your new pills look different - different color, shape, or imprint - that’s normal. But if you get a new batch that looks different from your last refill, ask the pharmacist. Verify the National Drug Code (NDC) on the bottle matches what you were prescribed. You can look up your NDC on the FDA’s Orange Book to see which generics are rated as therapeutically equivalent. If your pharmacy switches the generic brand without telling you - which happens often - that’s legal. But you have the right to ask for the same manufacturer each time. If you’ve had a good experience with one generic, request it by name. Many pharmacies will honor that.When to Call Your Doctor
Most changes are minor. But here’s when to act:- New or worsening side effects (rash, dizziness, nausea, confusion)
- Loss of symptom control (more seizures, higher blood pressure, unstable blood sugar)
- Unexplained fatigue or mood changes lasting more than two weeks
- Any change that makes you feel like you did before your condition was under control
Don’t wait. Don’t assume it’s “just in your head.” Your experience is valid. The FDA’s MedWatch program exists so patients can report problems. If you notice something unusual, report it. You’re helping improve safety for everyone.
What the Data Really Says
Let’s cut through the noise. In 2022, the FDA received over 1.2 million adverse event reports. Only about 15% involved generic drugs. Of those, less than 1% were confirmed as true therapeutic failures. On PatientsLikeMe, 92.7% of 42,000 people who switched to generics reported no loss of symptom control. Consumer Reports found 89% of users were satisfied. The bottom line? For the vast majority, generics work just as well. But that 3-7% who do notice a difference? Their stories matter. That’s why monitoring isn’t about distrust - it’s about personalization. Medicine isn’t one-size-fits-all. Even if the science says two pills are the same, your body might respond differently. That’s why your awareness, tracking, and communication with your doctor are the most powerful tools you have.What to Do Next
If you just switched:- Write down the name of the generic and the manufacturer (check the bottle).
- Set a reminder for a follow-up with your doctor in 2-4 weeks.
- Start tracking your key health metrics - even if you feel fine.
- Don’t panic if you feel a little off. But don’t ignore it either.
- Ask your pharmacist: “Is this the same generic I got last time?”
If you’ve been on a generic for months and feel fine - great. Keep going. But if you’ve ever thought, “I used to feel better on the brand,” now’s the time to talk to your doctor. You might be one of the rare cases where the brand works better for you - and that’s okay. There’s no shame in needing the original. Your health isn’t a cost-cutting exercise. It’s your life.
Are generic medications really as effective as brand-name drugs?
Yes, for the vast majority of people. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove bioequivalence - meaning they deliver the same amount of medicine into your bloodstream at the same rate. Over 90% of prescriptions in the U.S. are generics, and studies show they work just as well for most conditions.
Which medications should I be extra careful about when switching to generics?
Be extra cautious with drugs that have a narrow therapeutic index - where small changes in blood levels can cause big effects. These include warfarin (blood thinner), levothyroxine (thyroid), phenytoin and lamotrigine (anti-seizure), digoxin (heart), and some antidepressants like bupropion. For these, your doctor may recommend closer monitoring, including blood tests within the first 30 days after switching.
Can I ask my pharmacy to always give me the same generic brand?
Yes. While pharmacies can switch between approved generic manufacturers, you have the right to request a specific brand. Ask your pharmacist to note your preference in your profile. If you’ve had a good experience with one version - say, Teva’s levothyroxine - you can ask for it by name. Many pharmacies will accommodate this, especially if you’ve had issues before.
What should I do if I think my generic medication isn’t working?
Don’t stop taking it. Contact your doctor right away. Keep a log of symptoms, dates, and any changes in how you feel. Bring your pill bottle - the NDC number helps identify the manufacturer. Your doctor may order a blood test or switch you back temporarily to confirm the issue. If it’s a real problem, report it to the FDA through MedWatch to help track safety trends.
How long should I monitor my health after switching to a generic?
For most people, 30 days is enough. But for high-risk medications like thyroid, seizure, or blood thinners, monitor for 60 to 90 days. This gives your body time to adjust and allows your doctor to see trends in lab results. If you’re stable after 90 days, you can reduce monitoring - but keep an eye out for any new changes.

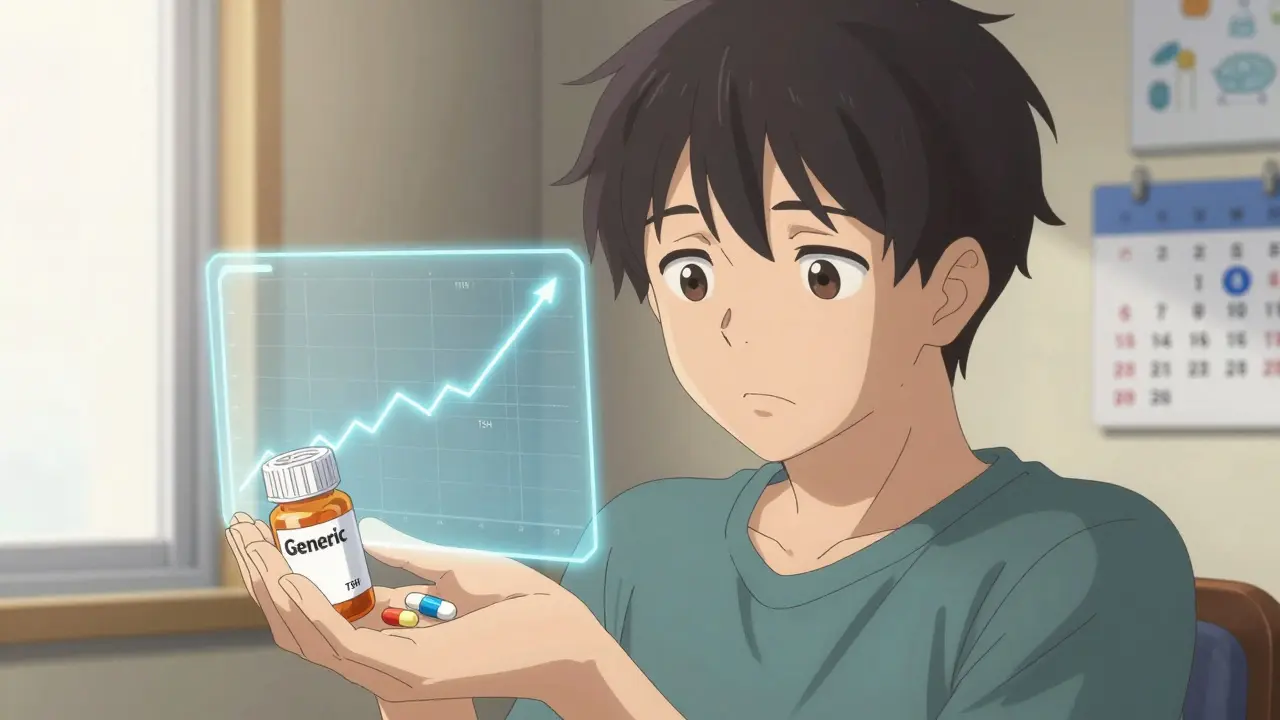
I switched to generic levothyroxine last year and didn’t think twice until I started feeling like a zombie at 3 p.m. Turns out my TSH jumped 15%. I kept a log, showed my doctor, and we adjusted the dose. No drama, no panic - just data. That’s all this post is asking for.