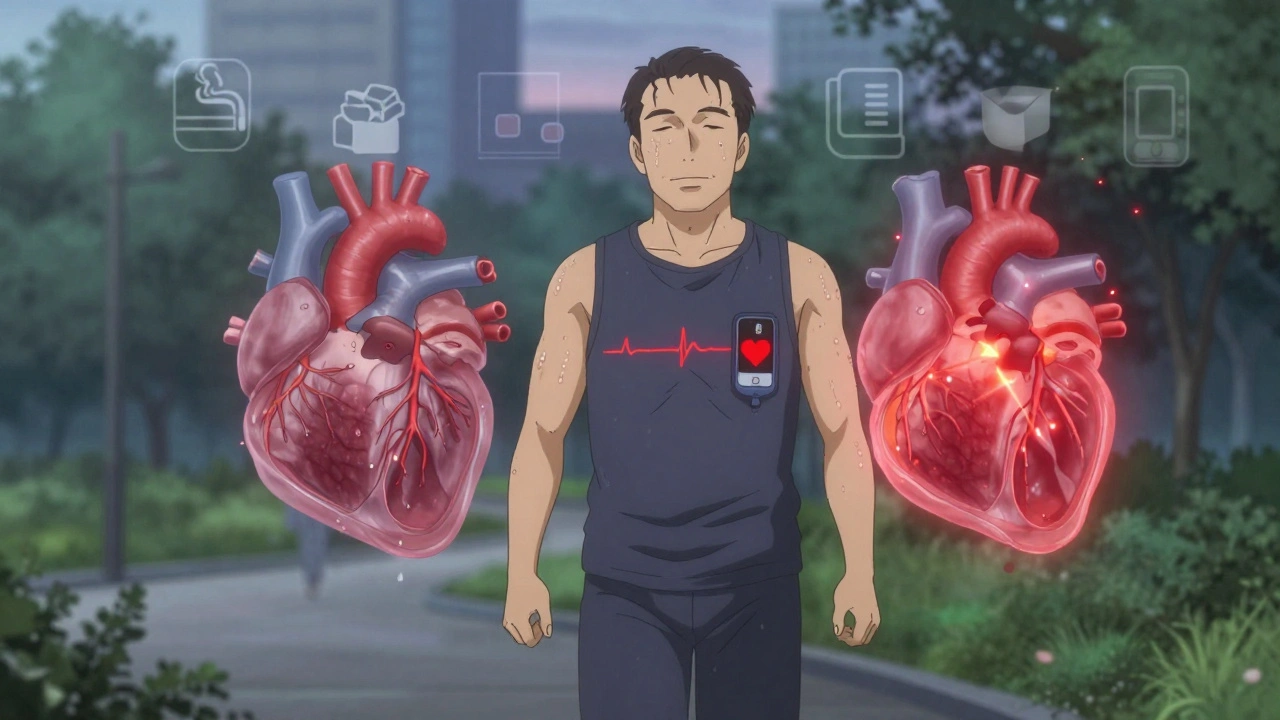
Coronary artery disease isn’t a sudden event. It’s a slow, silent process that starts decades before you feel any symptoms. By the time chest pain shows up, the arteries feeding your heart have already been clogged for years. This isn’t just about cholesterol-it’s about inflammation, lifestyle, and how your body responds to stress over time. And it’s the number one killer worldwide.
What Exactly Is Atherosclerosis?
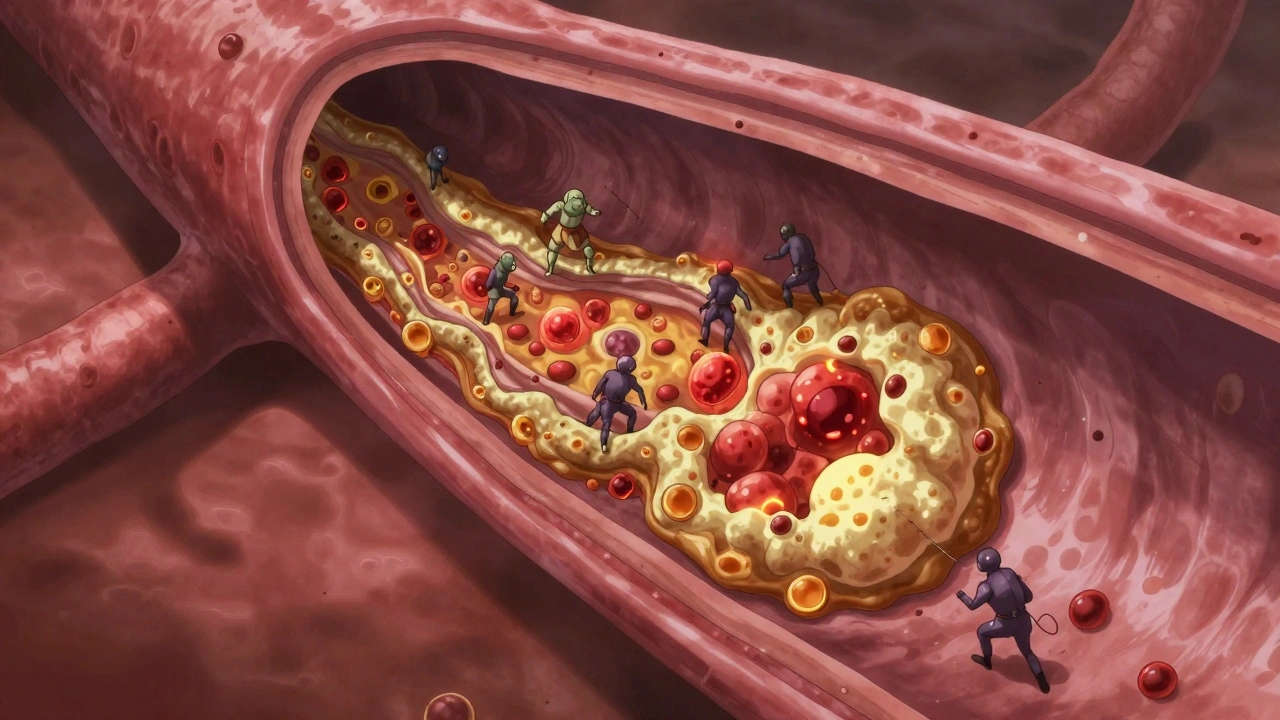
Atherosclerosis is the root cause of most coronary artery disease. It’s not just "plaque" in a vague, scary way-it’s a biological process where fatty deposits, cholesterol, calcium, and immune cells build up inside your artery walls. Think of it like rust forming inside a pipe, but instead of metal, it’s your blood vessels. Over time, these plaques harden and narrow the arteries, making it harder for blood to flow to your heart muscle.
Not all plaques are the same. Some are stable-thick, fibrous caps covering a large buildup. These can narrow arteries by more than 50%, causing predictable chest pain when you exercise. Others are unstable-soft, fatty cores with thin caps and lots of inflammation. These might only block 30% of the artery, but they’re dangerous because they can rupture without warning. When that happens, a blood clot forms on top, suddenly cutting off blood flow. That’s a heart attack.
What makes a plaque unstable? It’s not just size. High levels of LDL (bad) cholesterol, ongoing inflammation from smoking or diabetes, and high blood pressure all contribute. The body’s immune system tries to clean up the mess, but in doing so, it ends up making things worse. Macrophages swallow cholesterol, turn into foam cells, and trigger more inflammation. That’s why treating CAD isn’t just about lowering cholesterol-it’s about calming the inflammation too.
Who’s at Risk? The Real Culprits Behind CAD
Many people think only older, overweight smokers get coronary artery disease. That’s outdated. The risk factors are more nuanced-and more common-than you think.
High blood pressure is one of the biggest silent drivers. Every time your blood pushes too hard against artery walls, it damages the lining. That’s where plaque starts. High cholesterol, especially LDL above 130 mg/dL, feeds the process. But even if your cholesterol is "normal," if you have diabetes, your risk jumps dramatically. Diabetes doesn’t just raise blood sugar-it makes your blood vessels sticky and inflamed.
Smoking is still the most preventable cause. It doesn’t just damage your lungs. It directly harms your arteries, reduces oxygen in your blood, and makes clots more likely. Even secondhand smoke increases risk.
Obesity, especially belly fat, isn’t just about weight. It’s linked to insulin resistance, high triglycerides, and low HDL (good cholesterol). Family history matters too-if a close relative had a heart attack before 55 (men) or 65 (women), your risk is higher.
And here’s something many don’t realize: chronic kidney disease and atrial fibrillation are now recognized as major risk factors. If your kidneys aren’t filtering well, or your heart is beating irregularly, your chances of a heart event go up-even if you don’t have classic symptoms.
Doctors now classify risk into three levels: low (less than 1% chance of a heart event per year), intermediate (1-3%), and high (over 3%). About 60% of people with CAD fall into the high-risk group. And here’s the key: 75% of all heart attacks happen in this group. That means if you’re in the high-risk category, you need more than just a statin-you need a full plan.
How Is It Diagnosed? Beyond the ECG
Many people assume an ECG will catch CAD. It won’t-not always. A resting ECG can look perfectly normal even if your arteries are 80% blocked. That’s why diagnosis often needs more.
Stress tests are common. You walk on a treadmill while your heart rate, blood pressure, and ECG are monitored. If your heart doesn’t get enough blood during exertion, it shows up as changes on the monitor. But stress tests can miss blockages in smaller vessels, especially in women.
For a clear picture, doctors turn to coronary angiography. It’s invasive, but it’s the gold standard. A thin tube is threaded into your artery, dye is injected, and X-rays show exactly where blockages are. It’s not done lightly-it’s reserved for people with clear symptoms or high-risk profiles.
There’s also non-invasive options like CT angiography, which uses a scanner to create 3D images of your heart arteries. It’s great for ruling out disease, especially if you’re at low to moderate risk and have chest pain.
And don’t forget the ankle-brachial index (ABI). It’s a simple test that compares blood pressure in your ankle to your arm. If the numbers are off, it suggests you have blockages elsewhere-not just in your heart. About half of people with CAD also have peripheral artery disease. Treating one often means addressing the other.
Treatment: Lifestyle Isn’t Optional-It’s the Foundation
Medications help. Surgery helps. But nothing works long-term without lifestyle change. This isn’t a suggestion. It’s the baseline.
Start with diet. The Mediterranean diet isn’t a fad-it’s backed by decades of data. Focus on vegetables, fruits, whole grains, nuts, olive oil, and fish. Cut back on processed meats, sugary drinks, and refined carbs. You don’t need to go vegan. You just need to stop eating like a fast-food customer.
Exercise isn’t about running marathons. Just 150 minutes a week of brisk walking lowers your risk by 30%. That’s 30 minutes, five days a week. If you’re out of shape, start with 10-minute walks. Build up. Movement improves blood flow, lowers blood pressure, and reduces inflammation.
Quit smoking. Period. There’s no safe level. Within a year of quitting, your heart attack risk drops by half. After five years, it’s close to that of someone who never smoked.
Weight loss-even 5-10% of your body weight-can reverse insulin resistance, lower blood pressure, and improve cholesterol. You don’t need a gym membership. Just move more and eat less junk.
Medications: What’s Actually Needed?
Not everyone needs every drug. But most people with CAD will take at least one or two long-term.
Statins are the cornerstone. They don’t just lower LDL-they stabilize plaques and reduce inflammation. Even if your cholesterol is "normal," statins are often recommended for high-risk patients. Common ones include atorvastatin and rosuvastatin.
Aspirin is used in some cases to prevent clots, but it’s not for everyone. The risks of bleeding must be weighed against benefits. If you’ve had a heart attack or stent, you’ll likely take it. If you’re at risk but haven’t had an event, your doctor will decide.
Beta-blockers slow your heart rate and lower blood pressure. They’re often used after a heart attack to reduce strain. ACE inhibitors or ARBs help if you have high blood pressure, diabetes, or heart failure. They protect your kidneys and your heart.
For people with diabetes, SGLT2 inhibitors and GLP-1 agonists aren’t just for blood sugar-they’ve been shown to reduce heart attacks and hospitalizations for heart failure. These are now standard in many guidelines.
Procedures: When You Need More Than Pills
If lifestyle and meds aren’t enough, or if you’re having chest pain that won’t go away, procedures come in.
Percutaneous coronary intervention (PCI) is the most common. A balloon is inflated in the blocked artery, and a metal mesh stent is placed to keep it open. It’s quick, often done as an outpatient. But it’s not a cure. The artery can re-narrow if you don’t change your habits.
Coronary artery bypass grafting (CABG) is surgery. A vein or artery from another part of your body is used to create a detour around the blockage. It’s more invasive, but it’s the best option for people with multiple blockages, especially if they have diabetes. Long-term survival is better with CABG in these cases.
Neither procedure fixes the underlying disease. That’s why both require lifelong medication and lifestyle changes afterward. Skipping these means the new stent or bypass can fail too.
The Future: Personalized Care and Cardio-Oncology
The 2023 guidelines from the American Heart Association and American College of Cardiology emphasize one thing: personalization. There’s no one-size-fits-all plan. Your treatment should match your risk level, other conditions, and goals.
For example, if you have cancer and CAD, you need a different approach. Chemotherapy can damage your heart. Radiation can scar your arteries. That’s why cardio-oncology is growing fast-specialists now work together to manage both conditions safely.
Research is also looking at new drugs that target inflammation directly. Canakinumab, for instance, showed a 15% reduction in heart attacks in trials, even without lowering cholesterol. That’s huge. It proves inflammation is a target, not just a side effect.
And genetic testing? It’s not routine yet, but for people with early heart disease and no obvious risk factors, it can uncover inherited conditions like familial hypercholesterolemia. That changes everything.
What You Can Do Today
You don’t need to wait for symptoms. If you’re over 40, or have any risk factors, get checked. Blood pressure, cholesterol, and blood sugar are easy tests. Ask your doctor about your 10-year risk score.
Start small. Swap soda for water. Take the stairs. Walk after dinner. Quit smoking-even if you’ve tried before. Most people need multiple attempts. It’s not weakness. It’s human.
Coronary artery disease isn’t your fate. It’s a signal. A warning that your body needs better care. The good news? You can change it. Not overnight. But step by step, day by day.
Can you reverse coronary artery disease?
Yes, to some extent. While scarred arteries don’t fully disappear, plaque can shrink and stabilize with aggressive lifestyle changes and medications. Studies show that lowering LDL below 70 mg/dL and maintaining healthy blood pressure can reduce plaque volume over time. The goal isn’t to erase it, but to make it stable and less likely to rupture.
Do all plaques cause chest pain?
No. Stable plaques that narrow arteries by more than 50% often cause predictable chest pain during exercise-called stable angina. But unstable plaques, which are more dangerous, usually narrow the artery by less than 50% and cause no symptoms until they rupture. That’s why so many heart attacks come out of nowhere.
Is coronary artery disease only a problem for men?
No. Women are just as likely to die from it, but their symptoms are often different. Instead of crushing chest pain, women may feel fatigue, nausea, jaw pain, or shortness of breath. These are easily mistaken for stress or the flu. That’s why women are more likely to be misdiagnosed and have worse outcomes.
Can you have heart disease with normal cholesterol?
Absolutely. Cholesterol is just one piece. Inflammation, high blood pressure, diabetes, smoking, and genetics all play major roles. Many people with "normal" LDL still develop blockages because their arteries are inflamed or damaged by other factors. That’s why doctors now look at overall risk, not just one number.
What’s the difference between a heart attack and cardiac arrest?
A heart attack is a circulation problem-a blocked artery starves part of the heart muscle of oxygen. You’re usually awake and in pain. Cardiac arrest is an electrical problem-the heart stops beating entirely. You lose consciousness instantly. A heart attack can trigger cardiac arrest, but they’re not the same thing. Both are emergencies.
What If You’ve Already Had a Heart Attack?
If you’ve had one, your risk of another is high-especially in the first year. But it’s not inevitable. Lifelong medication is non-negotiable. Statins, beta-blockers, aspirin, and sometimes newer drugs like SGLT2 inhibitors are standard. Don’t skip doses. Don’t stop because you "feel fine."
Cardiac rehab is one of the most underused tools. It’s not just exercise. It’s education, counseling, nutrition support, and peer support. People who complete rehab cut their risk of another event by 25-30%. Yet only about half of eligible patients enroll.
And don’t ignore mental health. Depression after a heart attack is common-and it doubles your risk of death. Talk to someone. Therapy, support groups, even medication can make a difference.
Coronary artery disease isn’t a life sentence. It’s a challenge. And with the right plan, you can live a full, active life-even with blocked arteries.

So basically if you eat a donut you're gonna die? Cool thanks for the fearmongering lol