When you fill a prescription for high blood pressure or cholesterol, chances are you’re getting a generic drug. In fact, cardiovascular generics make up nearly one in every three pills prescribed in the U.S. They’re cheaper, widely available, and approved by the FDA. But do they work the same? Are they safe? And why do some patients and doctors still hesitate?
What Exactly Are Cardiovascular Generics?
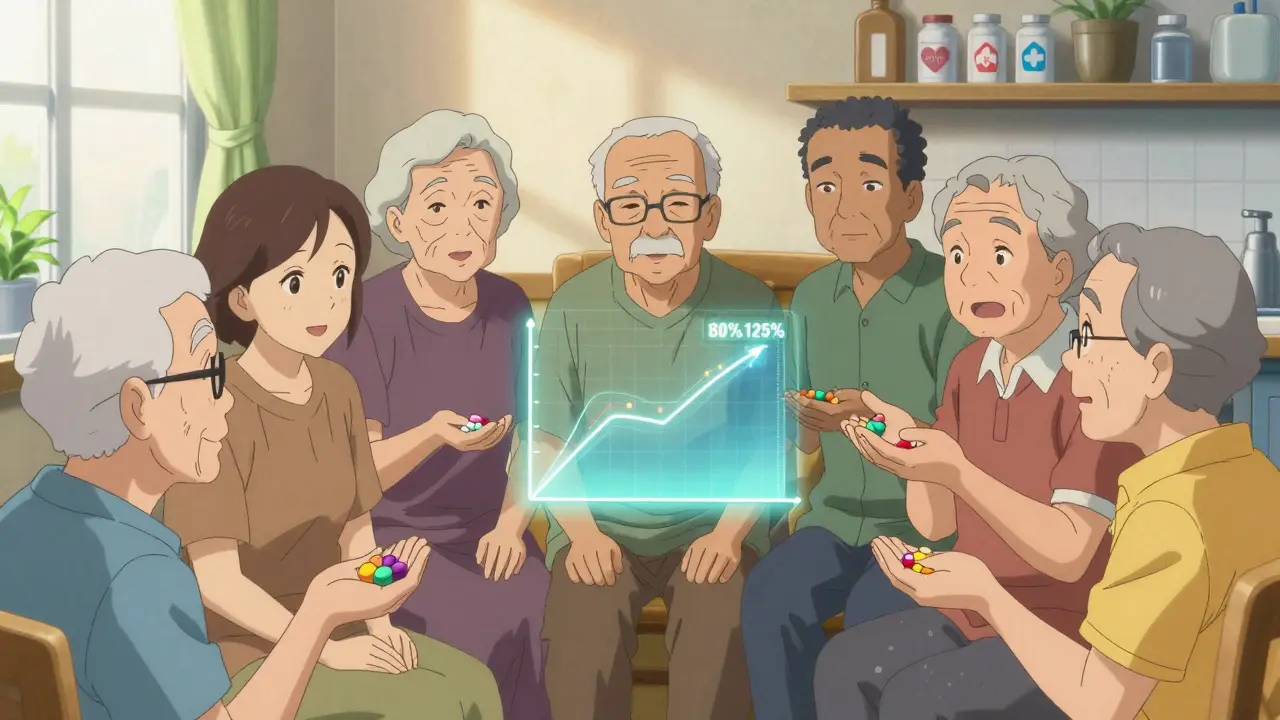
Cardiovascular generics are exact chemical copies of brand-name heart and blood pressure drugs like lisinopril, atorvastatin, or metoprolol. Once the original patent expires, other manufacturers can produce the same active ingredient. The FDA doesn’t require them to repeat expensive clinical trials. Instead, they must prove bioequivalence: their version gets into the bloodstream at the same rate and amount as the brand-name drug. The standard? The amount of drug absorbed must fall within 80% to 125% of the brand’s levels - a tight range that’s been used since the 1980s.
This isn’t just theory. In 2021, the FDA found that on average, generics differed from brand-name versions by just 3.5% in absorption. That’s less than the natural variation your body shows from day to day. For most people, that’s not a problem.
Do Generics Work as Well as Brand Names?
A 2020 Harvard Health meta-analysis looked at 38 high-quality studies comparing generic and brand-name cardiovascular drugs. In 35 of them - 92.1% - outcomes were identical. Patients had the same blood pressure control, same cholesterol reduction, same number of heart attacks or strokes. The other three showed tiny differences, but nothing that changed how patients felt or what happened to them clinically.
Another large 2023 review, analyzing data from over a million patients, found no meaningful difference in major heart events like heart attacks or death between generics and brand names. The overall risk ratio? 1.02 - meaning virtually no difference.
But here’s where it gets complicated. The same review found that for statins, generics showed a slightly higher risk of major heart events (risk ratio 1.13). For calcium channel blockers, generics had fewer adverse events (0.90). Why? It’s not because the active ingredient is weaker. It’s likely because of differences in inactive ingredients - things like fillers, dyes, or coatings - that affect how the pill breaks down in your stomach.
The Quebec Study: When Switching Causes Problems
In 2019, researchers in Quebec tracked over 136,000 seniors after generic versions of ARBs (like losartan and valsartan) became available. In the first month after switching, adverse events jumped: 8% for losartan, 11.7% for valsartan, and 14% for candesartan. That’s a big jump from the pre-generic rate of 10%.
What happened? The drugs were still bioequivalent. The active ingredient was the same. But patients were suddenly on pills with different colors, shapes, or coatings. Some patients didn’t recognize the new pill. Others had stomach upset from a new filler. Some stopped taking it altogether. The study didn’t say generics were unsafe - it said switching without support caused problems.
Dr. Paul Poirier, one of the study’s authors, put it simply: “The issue isn’t the drug. It’s the transition.”
Why Do Some Doctors Still Prefer Brand Names?
Even with all the data, nearly a quarter of physicians say they wouldn’t use generics for their own families. Why? Two reasons: perception and experience.
Many doctors remember the 2018-2020 nitrosamine recalls. Contaminated valsartan, losartan, and irbesartan generics were pulled from shelves after being linked to cancer-causing impurities. Over 1,200 lots were recalled. That shook trust - even though the problem was manufacturing, not the generic model itself.
Another issue: pill appearance. A 2019 JAMA study found that when patients got a new generic version with a different color or shape, 14.2% stopped taking their medication. That’s not because the drug didn’t work - it’s because they thought it was the wrong pill.
And then there’s the gap between data and belief. A 2023 Consumer Reports survey found 61% of Americans think brand-name drugs are more effective. Even though studies show otherwise, the idea sticks.
Who’s Most at Risk?
Not everyone has the same experience with generics. Some groups need extra care:
- Older adults: More likely to take multiple meds, more sensitive to pill changes, more likely to stop if confused.
- Patients on narrow therapeutic index drugs: Like warfarin or digoxin. Small changes in blood levels can cause serious effects. The American Heart Association advises against automatic substitution without monitoring.
- People with chronic conditions: If you’ve been stable on a brand-name drug for years, switching for cost alone might not be worth the risk of disruption.
Statins are the most common cardiovascular generic - and the most studied. Their generic market share is 94.3%. For most people, switching to generic statins saves hundreds a year with no loss in protection. But for those who’ve had a heart attack or stroke, some doctors still recommend staying on brand - not because generics don’t work, but because they want to minimize any possible disruption.
Manufacturing and Quality: Are Generics Safe?
Generics must follow the same strict manufacturing rules as brand-name drugs: Current Good Manufacturing Practices (cGMP). But here’s the catch: in 2022, the FDA found that 12.7% of generic drug facilities had critical deficiencies. That’s higher than the rate for brand-name makers.
Most of these issues were paperwork errors or cleaning protocols - not dangerous contamination. But the 2018 nitrosamine crisis showed what can go wrong when oversight slips. Since then, the FDA has tightened controls. In 2024, they began unannounced inspections targeting cardiovascular generics. Of the first 100 facilities inspected, nearly half (47.3%) had findings - up from 32% under normal inspections.
Today, manufacturers must test for nitrosamines at levels as low as 96 nanograms per day. That’s less than a grain of salt in a swimming pool. But it’s enough to trigger a recall if missed.
What About Cost and Access?
Cardiovascular generics saved the U.S. healthcare system $300 billion between 2010 and 2019. That’s about 18% of all generic savings. Without them, millions of people couldn’t afford to take their blood pressure or cholesterol meds.
Medicare Part D plans now use generics in nearly 90% of cardiovascular prescriptions. Commercial insurers are slower - only 76% - but they’re catching up. The average cost for a 30-day supply of generic atorvastatin? $4. Brand-name Lipitor? Over $200.
Cost isn’t just about the pill. It’s about adherence. Studies show patients on generics are more likely to take their meds regularly because they can afford them. That’s a bigger win than any small difference in bioequivalence.
What Should You Do?
If you’re on a brand-name cardiovascular drug and your doctor suggests switching to generic:
- Ask if your drug is on the list of those with proven equivalent outcomes (most are).
- Check if your current pill has changed color, shape, or size - and ask your pharmacist to explain why.
- Don’t stop taking it if you feel different. Call your doctor or pharmacist. It might be a temporary adjustment.
- If you’re on warfarin, digoxin, or another narrow-therapeutic-index drug, insist on monitoring after any switch.
- Use a pill organizer. It helps you notice if something’s changed.
For most people, generic cardiovascular drugs are safe, effective, and life-saving. The evidence is clear. But trust isn’t built on data alone. It’s built on communication, consistency, and care.
What’s Next for Cardiovascular Generics?
More generics are coming. New drugs like sacubitril/valsartan (Entresto) will lose patent protection soon. But these are complex molecules - harder to copy than simple pills. The FDA is already preparing new testing rules for these next-generation generics.
The European Medicines Agency has already required new food-effect studies for generic rivaroxaban. That means future generics will be tested not just in fasting patients, but also after meals - a more real-world test.
For now, the message is simple: Generics work. But they’re not all the same. The key isn’t brand or generic - it’s knowing your drug, your body, and your care team.
Are generic cardiovascular drugs as safe as brand-name drugs?
For most people, yes. Large studies show that 90%+ of generic cardiovascular drugs perform just as well as brand names in controlling blood pressure, cholesterol, and preventing heart events. The FDA requires them to meet strict bioequivalence standards. However, rare cases of increased adverse events have been seen right after switching - often due to changes in pill appearance or inactive ingredients, not the active drug itself.
Why do some patients have more side effects after switching to generics?
It’s usually not the active ingredient. Side effects after switching often come from changes in fillers, dyes, or coatings that affect how the pill dissolves. Some patients are sensitive to these differences. Others stop taking the medication because they don’t recognize the new pill. A 2019 study found a 14.2% increase in discontinuation when pill appearance changed. That’s why pharmacist counseling and consistent pill appearance matter.
Is there a difference between generic statins and brand-name statins?
Most studies show no difference. But one major 2023 analysis found a small but statistically significant increase in major heart events with generic statins (risk ratio 1.13). The reason isn’t clear - it could be formulation differences, patient adherence, or even random variation. For most people, the cost savings far outweigh this tiny risk. But if you’ve had a recent heart attack or are on high-dose statins, talk to your doctor before switching.
Should I avoid generics if I’m on warfarin or digoxin?
Yes, proceed with caution. These drugs have a narrow therapeutic index - meaning small changes in blood levels can cause serious harm. The American Heart Association recommends against automatic substitution. If you switch, your doctor should monitor your blood levels closely for several weeks. Don’t switch without supervision.
Can I trust the quality of generic drugs made overseas?
The FDA inspects all facilities - whether in the U.S., India, or China - using the same standards. In 2022, 12.7% of generic drug plants had critical deficiencies. That’s higher than for brand-name makers, but most issues were paperwork or cleaning errors, not dangerous contamination. The 2018 nitrosamine crisis led to stricter testing, and the FDA now does unannounced inspections on cardiovascular generics. If your drug is FDA-approved, it meets U.S. safety standards.
Why do some doctors still prefer brand-name drugs?
Some doctors are influenced by past recalls, patient complaints, or outdated beliefs. Even though evidence shows generics are safe, nearly 25% of physicians say they wouldn’t use them for their own families. That’s largely due to perception, not science. The American College of Physicians found that half of medical journal commentaries on generics expressed hesitation - even when the data supported them.

Look, I don't care what the FDA says-I’ve seen people crash after switching to generics. My uncle went from 120/80 to 170/105 in two weeks. They changed the filler, he didn’t know, and now he’s on three meds instead of one. This isn’t science-it’s a cost-cutting gamble with people’s lives.