When you have diabetes, your kidneys are under constant stress. Over time, high blood sugar damages the tiny filters in your kidneys, letting protein leak into your urine. This is called diabetic nephropathy-and it’s the leading cause of kidney failure in people with diabetes worldwide. But here’s the good news: we know exactly how to slow it down. Two types of blood pressure medicines-ACE inhibitors and ARBs-along with tight control of protein in the urine, can make a real difference. Not just a small one. A life-changing one.
What Diabetic Nephropathy Really Means
Diabetic nephropathy isn’t just high blood pressure or a little protein in the urine. It’s a specific kidney injury caused by long-term diabetes. The diagnosis usually comes when you have persistent albuminuria-more than 30 mg of albumin per gram of creatinine in your urine-measured on two tests at least three months apart. This isn’t a one-off result. It’s a warning sign your kidney filters are breaking down.
And it’s not just about kidney health. People with diabetic nephropathy have a much higher risk of heart attacks, strokes, and early death. The damage to the kidneys doesn’t happen in isolation. It’s tied to the same blood vessel problems that cause heart disease. That’s why treating it isn’t optional-it’s essential.
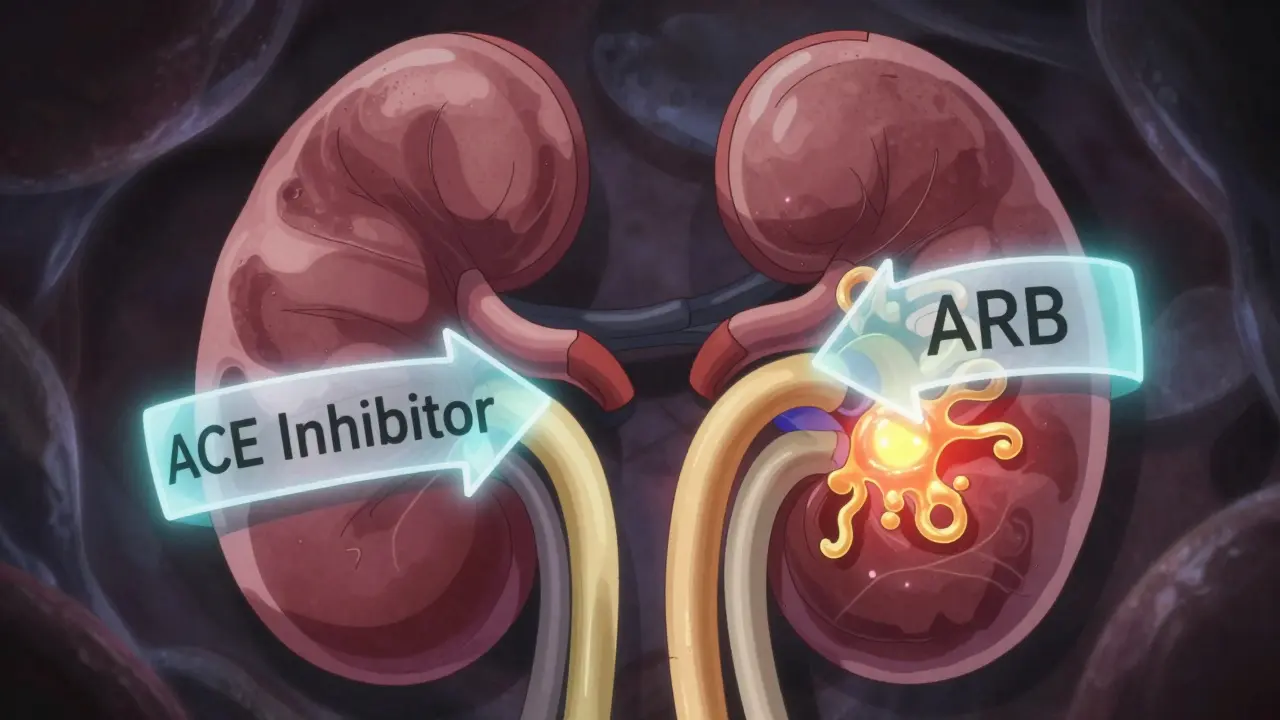
Why ACE Inhibitors and ARBs Are First-Line Treatment
For over 20 years, ACE inhibitors and ARBs have been the go-to medications for diabetic nephropathy. Why? Because they do more than lower blood pressure. They directly protect the kidneys.
Both drugs block the renin-angiotensin-aldosterone system (RAAS)-a hormone pathway that tightens blood vessels and increases pressure inside the kidney’s filtering units. High pressure in these tiny filters is what forces protein out into the urine. By relaxing those vessels, ACE inhibitors and ARBs reduce that pressure. Less pressure means less protein leakage. And less protein leakage means slower kidney damage.
Large studies like the RENAAL and IDNT trials showed that ARBs like losartan and irbesartan cut the risk of kidney failure by up to 30% in people with type 2 diabetes and heavy proteinuria. ACE inhibitors like captopril and ramipril showed similar results in type 1 diabetes. These aren’t small effects. These are the kinds of results that change clinical guidelines.
Protein Control Isn’t Optional-It’s the Goal
Doctors don’t just prescribe these drugs to lower blood pressure. They prescribe them to reduce proteinuria. That’s the real marker of success.
If your urine albumin-to-creatinine ratio (UACR) is above 300 mg/g, you’re in the high-risk zone. That’s when guidelines say you need the highest tolerated dose of an ACE inhibitor or ARB. Not half a dose. Not a low dose you’ve been on for years. The full, maximum dose that your body can handle.
Here’s the catch: most patients never get there. Many doctors stop increasing the dose if the creatinine level rises a little-even if it’s under 30%. But that rise isn’t kidney damage. It’s a normal side effect of the drug working. Lowering the pressure inside the kidney temporarily reduces blood flow, which raises creatinine. That’s not a reason to stop. It’s a sign you’re on the right track.
Ignoring this leads to suboptimal care. And that’s why only about 60-70% of eligible patients get the right dose. We’re leaving protection on the table.
Dosing Matters-Here’s What Works
Not all ACE inhibitors and ARBs are dosed the same. And not all are used the same way in diabetic nephropathy.
- Captopril: The only ACE inhibitor with FDA approval specifically for diabetic nephropathy. Dose: 25 mg three times daily.
- Ramipril: Often started at 2.5-5 mg once daily, up to 20 mg daily for kidney protection.
- Benazepril: Start at 10 mg once daily, increase to 20-40 mg daily.
- Losartan: ARB used in RENAAL trial. Dose: 50-100 mg daily.
- Irbesartan: Used in IDNT trial. Dose: 150-300 mg daily.
These aren’t guesses. These are the doses used in the trials that proved effectiveness. If you’re on half of that, you’re not getting the full benefit.

Why You Shouldn’t Combine ACE Inhibitors and ARBs
You might think, “If one is good, two must be better.” That’s not true here.
Trials like VA NEPHRON-D, ONTARGET, and ALTITUDE tested combining ACE inhibitors with ARBs-or adding a direct renin inhibitor like aliskiren. The results? No extra kidney protection. But a big spike in side effects.
Patients on dual RAAS blockade had twice the risk of acute kidney injury and three times the risk of dangerously high potassium levels (hyperkalemia). That’s not a trade-off worth making. The risks outweigh the benefits. Every major guideline now says: pick one. Use it at the highest tolerated dose. Don’t double up.
What About Other Blood Pressure Drugs?
ACE inhibitors and ARBs are the foundation. But you might need more to reach your blood pressure goal.
Guidelines from the American Diabetes Association say it’s fine-and often necessary-to add:
- Diuretics (like hydrochlorothiazide)
- Calcium channel blockers (like amlodipine)
- Beta blockers (like metoprolol)
These help control blood pressure when RAAS blockers alone aren’t enough. But they don’t replace them. They support them.
One big warning: avoid NSAIDs like ibuprofen or naproxen if you’re on an ACE inhibitor or ARB. Together, they can cause sudden kidney failure-especially if you’re also on a loop diuretic like furosemide. That combo is a recipe for trouble.
The New Players: SGLT2 Inhibitors and MRAs
It’s 2026. We’ve got new tools. SGLT2 inhibitors (like empagliflozin, dapagliflozin) and nonsteroidal mineralocorticoid receptor antagonists (like finerenone) are now part of the conversation.
But here’s the key: every major trial proving their benefit was done in patients already taking an ACE inhibitor or ARB-at maximum tolerated doses. That’s not an accident. It means these newer drugs work best on top of the foundation, not instead of it.
If you can’t tolerate an ACE inhibitor or ARB due to cough or swelling, then yes, an SGLT2 inhibitor becomes your first choice for kidney protection. But if you can take them? Start with them. Then add the new ones.

Who Shouldn’t Get These Drugs?
Not everyone with diabetes needs an ACE inhibitor or ARB.
Guidelines are clear: don’t use them for primary prevention in people with normal blood pressure and no protein in their urine. A study of normotensive type 1 diabetics with normal albumin levels showed enalapril didn’t slow kidney damage-though it did help with eye complications. So no, you don’t need it just because you have diabetes.
These drugs are for people who are hypertensive, proteinuric, or both. That’s the target group. Don’t overprescribe. But don’t underprescribe either.
The Real Problem: Underuse and Underdosing
Here’s the uncomfortable truth: we’re failing many patients.
Studies show that even after a diagnosis of chronic kidney disease, nearly 40% of people with diabetes never start an ACE inhibitor or ARB. Of those who do, most are on doses far below what the trials used.
Why? Fear. Fear of rising creatinine. Fear of high potassium. Fear of side effects. But the data says: don’t stop. Don’t hold back. The benefits are real. The risks are manageable. And the cost of inaction? Kidney failure. Dialysis. Early death.
Maximizing these drugs isn’t optional. It’s the standard of care.
What You Can Do
If you have diabetes and kidney damage:
- Ask if you’re on an ACE inhibitor or ARB.
- If you are, ask what dose you’re on-and whether it’s the maximum tolerated dose.
- If your creatinine rose a little after starting the drug, ask if that’s expected. Don’t assume it’s a problem.
- Ask about avoiding NSAIDs and loop diuretics unless absolutely necessary.
- Ask if you’re a candidate for an SGLT2 inhibitor or finerenone-on top of your RAAS blocker.
This isn’t about taking more pills. It’s about taking the right ones, at the right doses, for the right reasons.
Can ACE inhibitors or ARBs reverse diabetic nephropathy?
They can’t reverse existing damage, but they can significantly slow or even stop further progression. Many patients stabilize their kidney function and avoid dialysis for years-or decades-when these drugs are used correctly at high doses.
Why do ACE inhibitors cause a cough?
ACE inhibitors block the breakdown of bradykinin, a substance that can irritate the throat and trigger a dry, persistent cough in about 10-20% of users. If this happens, switching to an ARB usually resolves the cough, since ARBs don’t affect bradykinin.
Is it safe to take an ACE inhibitor or ARB if I have low blood pressure?
Yes, if you have proteinuria and diabetic nephropathy. These drugs protect your kidneys even if your blood pressure is normal or low. The goal isn’t just to lower BP-it’s to reduce pressure inside the kidney’s filters. Many patients with normal BP still benefit from these medications if they have albuminuria.
How often should I get my urine and blood tested?
When starting or adjusting an ACE inhibitor or ARB, check your serum creatinine and potassium within 1-2 weeks. After that, test your urine albumin-to-creatinine ratio (UACR) every 3-6 months and your blood tests every 6 months. More frequent testing may be needed if you’re on diuretics or have advanced kidney disease.
Can I stop taking these drugs if my proteinuria improves?
No. Even if your urine protein drops to normal, you should continue the medication. The protective effect is ongoing. Stopping increases the risk of disease progression. These drugs are typically taken long-term, often for life, unless side effects become intolerable.
What if I can’t afford these medications?
Many generic versions are available and cost under $10 per month in most countries. If cost is a barrier, talk to your doctor or pharmacist about alternatives. Some manufacturers offer patient assistance programs. Never skip doses because of cost-this is one of the most cost-effective kidney-protective treatments available.
Final Thought: Don’t Settle for Less
Diabetic nephropathy doesn’t have to mean dialysis. It doesn’t have to mean early death. We have the tools. We know how to use them. The science is clear. The guidelines are solid.
The problem isn’t lack of knowledge. It’s lack of action. Too many patients are on too-low doses. Too many are never started at all. Too many are told to stop because their creatinine went up-and they never get back on.
If you have diabetes and kidney damage, you deserve the best protection we have. That means ACE inhibitors or ARBs at the highest dose you can tolerate. Not less. Not later. Now.

Man, I wish my doc talked like this. I’ve been on ramipril for two years but never knew I should be pushing the dose higher. Just glad I found this-thanks for laying it out so clearly.