GLP-1 Weight Loss Calculator
Weight Loss Calculator
Estimate potential weight loss with GLP-1 agonists based on your current weight and medication type.
Results
When you think of diabetes medications, you probably picture pills that lower blood sugar. But today, some of the most talked-about drugs in medicine aren’t just helping people with diabetes-they’re reshaping how we treat obesity, heart disease, and even mental health. The reason? GLP-1 agonists. These aren’t new, but what they can do now goes far beyond what anyone expected when the first one hit the market in 2005.
What Are GLP-1 Agonists, Really?
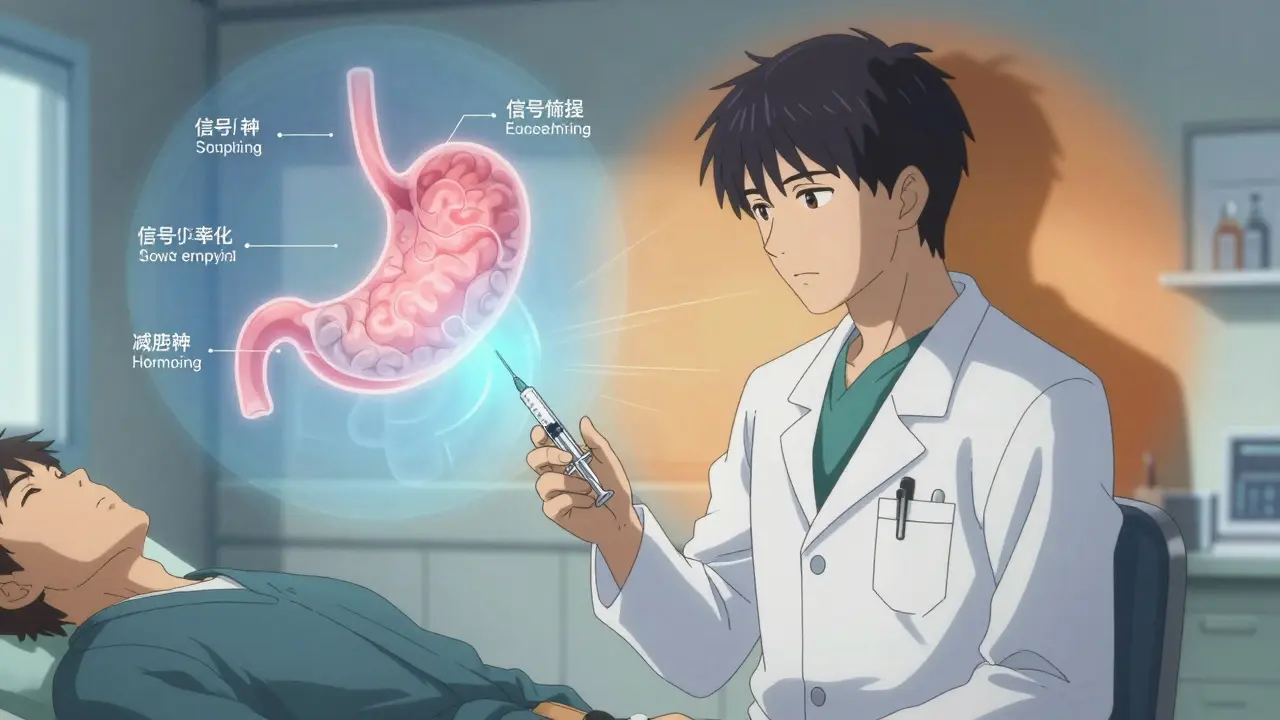
GLP-1 agonists are synthetic versions of a hormone your body makes naturally called glucagon-like peptide-1. This hormone does three big things: it tells your pancreas to release insulin when blood sugar rises, it stops your liver from pumping out too much glucose, and it slows down how fast food leaves your stomach. But here’s the twist-it also sends a signal to your brain that says, "You’re full."
That last part? It’s why people lose weight. You don’t feel hungry the same way. Snacks lose their pull. Binge eating becomes harder. The result? People eat less, without fighting cravings or counting calories.
Today’s versions-like semaglutide (Ozempic, Wegovy), tirzepatide (Mounjaro, Zepbound), and liraglutide (Victoza, Saxenda)-are far more powerful than the first ones. Semaglutide and tirzepatide, in particular, have turned heads. In clinical trials, tirzepatide helped people lose up to 20% of their body weight. That’s not a few pounds. That’s like dropping a whole suitcase of extra weight.
Weight Loss That Actually Sticks (For a While)
Most diets fail. People lose weight, then gain it back. But GLP-1 agonists? They change the game. In the STEP-1 trial, people using semaglutide 2.4 mg weekly lost nearly 15% of their body weight over 68 weeks. Compare that to the placebo group, who lost just 2.4%. The difference isn’t subtle-it’s dramatic.
And it’s not just about the scale. In people with type 2 diabetes and obesity, tirzepatide led to an average 11.6% weight loss over 72 weeks. That’s with a starting weight of over 100 kg. These numbers aren’t outliers-they’re consistent across studies.
But here’s what most people don’t talk about: the weight comes back fast if you stop. Clinical data shows that within a year of stopping, 50-70% of the lost weight returns. That’s not a flaw-it’s a feature of how the drug works. It doesn’t reprogram your metabolism. It suppresses appetite while you’re taking it. Once you stop, your body goes back to its old patterns. That’s why experts say these drugs work best as part of a longer-term plan, not a quick fix.
Beyond Weight: The Hidden Health Wins
Let’s be clear-GLP-1 agonists aren’t just weight-loss drugs. They’re multi-tool medications. A 2024 study in Nature Cardiovascular Research found that people taking these drugs had 12-18% fewer heart attacks, strokes, and heart-related deaths. That’s huge. For someone with diabetes and high blood pressure, this isn’t a bonus-it’s life-saving.
They also lower blood pressure. Reduce bad cholesterol (LDL). Improve triglyceride levels. One study even showed a 14% drop in suicidal thoughts among users compared to those on older diabetes meds. That’s not a side effect. That’s a therapeutic benefit.
And it gets weirder. A 2024 study of 2 million U.S. veterans found GLP-1 users had a 23% lower chance of seizures, a 17% lower risk of substance addiction (including alcohol and opioids), and even a 11% drop in schizophrenia diagnoses. The science isn’t fully understood yet, but the brain clearly responds to these hormones. Some researchers think GLP-1 receptors in the brain help calm overactive neural circuits.
Who Gets the Most Benefit?
These drugs aren’t magic for everyone. They work best in people with:
- Type 2 diabetes and obesity
- Prediabetes with excess weight
- Heart disease and high BMI
- High triglycerides or fatty liver disease
For someone with a BMI over 30 and insulin resistance? These drugs can be transformative. But for a lean person with no metabolic issues? The weight loss is small, and the side effects might not be worth it.
And here’s a hard truth: they don’t work well without lifestyle changes. A 2024 review in Diabetes Care showed that people who combined semaglutide with nutrition counseling and movement lost 3x more weight than those who just took the drug. Exercise doesn’t make the drug work better-it makes the results last.
The Side Effects No One Talks About
Yes, these drugs help people lose weight. But they’re not gentle. About 30-50% of users get nausea, vomiting, or diarrhea. For some, it’s mild and fades after a few weeks. For others? It’s daily misery. On Reddit, 68% of users reported gastrointestinal distress severe enough to affect work or sleep.
Then there’s "Ozempic face." It’s not official medical jargon, but it’s real. Long-term users report loss of facial fat, hollow cheeks, and skin that looks older. Harvard Health documented this in 42% of users who’d been on the drug for over a year. It’s not dangerous-but it’s startling. And there’s no fix except stopping the drug.
There’s also the risk of pancreatitis (0.5-1% of users) and gallbladder issues. And while rare, the FDA requires warnings about possible thyroid tumors in rodents (no proven link in humans yet). That’s why these drugs are only for people who truly need them-not for cosmetic use.
Cost and Access: The Real Barrier
Wegovy costs $1,349 a month without insurance. That’s more than most people make in a week. Even with insurance, many plans don’t cover it for weight loss. In 2023, 58% of users in the U.S. reported insurance denials. Some people ration their doses-skipping weeks to stretch their supply. That’s dangerous. Dose escalation is built into the treatment plan for a reason. Skipping steps increases side effects and reduces effectiveness.
Novo Nordisk offers a program that covers 75% of out-of-pocket costs for eligible patients. But you need to qualify. Many don’t. That’s why only 2% of eligible Americans are on these drugs, even though 42% of U.S. adults have obesity.
Corporate America is stepping in. Amazon and Walmart added GLP-1 drugs to employee health plans in 2024. That’s a sign things are changing-but it’s still far from universal.
How These Drugs Compare
| Drug Name | Brand (Weight Loss) | Brand (Diabetes) | Dosing | Average Weight Loss | Cardiovascular Benefit |
|---|---|---|---|---|---|
| Tirzepatide | Zepbound | Mounjaro | Once weekly | 15-20% | Yes (15% reduction in events) |
| Semaglutide | Wegovy | Ozempic | Once weekly | 12-15% | Yes (18% reduction in events) |
| Liraglutide | Saxenda | Victoza | Once daily | 5-10% | Yes (13% reduction in events) |
| Dulaglutide | - | Trulicity | Once weekly | 4-8% | Yes (12% reduction in events) |
| Exenatide | - | Byetta | Twice daily | 2-5% | Moderate |
Tirzepatide is the strongest, followed by semaglutide. The older drugs still work, but they’re less effective and harder to stick with. Oral semaglutide (Rybelsus) is an option for those who hate needles, but it’s less potent and still costs over $900/month.
What’s Next?
The future is crowded. Novo Nordisk is testing a 50 mg oral semaglutide pill that could be taken once daily. Eli Lilly is developing triple agonists that hit GLP-1, GIP, and glucagon receptors at once-early data shows even bigger weight loss. Implants that last six months? In the lab.
But bigger isn’t always better. With more powerful drugs comes more risk. Will we see a rise in eating disorders? More cases of "Ozempic face"? Will insurers cover these at $2,000/month? The market is expected to hit $100 billion by 2030. But if only 10% of people can afford it, does that help society-or just the wealthy?
What Should You Do?
If you’re struggling with weight and have type 2 diabetes, prediabetes, or heart disease, talk to your doctor. These drugs can change your life. But they’re not a shortcut. They work best with:
- Gradual dose increases to avoid nausea
- Regular follow-ups with your provider
- Protein-rich meals and balanced carbs
- At least 150 minutes of movement per week
- Patience-results take months
If you’re healthy and just want to lose a few pounds? These aren’t for you. The risks outweigh the rewards. And if you’re on one? Don’t quit cold turkey. Work with your doctor to taper off slowly. Otherwise, you’ll likely regain the weight-and then some.
Are GLP-1 agonists safe for long-term use?
Yes, for people with obesity, diabetes, or heart disease, long-term use is considered safe. Clinical trials now extend beyond five years, with no new major safety signals emerging. However, side effects like nausea, gallbladder issues, and rare pancreatitis cases do occur. Regular monitoring by a healthcare provider is essential. The FDA requires ongoing safety studies for all approved GLP-1 agonists.
Can I take GLP-1 agonists if I don’t have diabetes?
Yes. Zepbound (tirzepatide) and Wegovy (semaglutide) are FDA-approved specifically for chronic weight management in adults with obesity or overweight (BMI ≥27) with at least one weight-related condition. These are not off-label uses-they’re approved indications. But you still need a prescription and medical oversight.
Why do GLP-1 agonists cause nausea?
They slow gastric emptying, which means food stays in your stomach longer. This can cause bloating, fullness, and nausea, especially when starting or increasing the dose. Most people adapt within 4-8 weeks. Starting at the lowest dose and increasing slowly reduces this risk. Drinking water, eating smaller meals, and avoiding fatty foods helps too.
Do GLP-1 agonists cure diabetes?
No. They help manage type 2 diabetes by improving blood sugar control and reducing insulin resistance. Some people achieve remission-meaning their HbA1c drops below 6.5% without meds-but this usually happens when weight loss is significant and maintained. If you stop the drug, blood sugar often rises again. They’re a powerful tool, not a cure.
Is there a pill version of GLP-1 agonists?
Yes. Rybelsus (oral semaglutide) is FDA-approved and taken daily. It’s less effective than the injectable version, with average weight loss around 7-8%. It’s also more expensive than some injectables. Newer oral versions with higher bioavailability are in Phase 3 trials and may be available by 2027.
GLP-1 agonists aren’t perfect. They’re expensive, they have side effects, and they’re not for everyone. But for millions of people with obesity and diabetes, they’re the most effective tool we’ve ever had. The future of weight management isn’t about willpower-it’s about biology. And for the first time, we’re finally matching science to need.

