Hypoglycemia Treatment Calculator
The 15-15 Rule Calculator
Calculate exactly how much fast-acting sugar you need to safely raise your blood sugar from low levels to a safe range (70 mg/dL or above).
Low blood sugar isn’t just an inconvenience-it can be dangerous. If you’re taking insulin, sulfonylureas, or meglitinides for diabetes, you’re at real risk of hypoglycemia. Blood glucose below 70 mg/dL triggers symptoms like shaking, sweating, and confusion. Below 54 mg/dL, you’re at risk of seizures or loss of consciousness. And it’s not rare: 1 in 3 insulin users experiences at least one severe low each year. The good news? You can manage it. Not with guesswork, but with a clear, practical plan built on real data and proven strategies.
Know Which Medications Put You at Risk
Not all diabetes drugs cause low blood sugar. Metformin, GLP-1 agonists like semaglutide, and SGLT2 inhibitors like empagliflozin carry very low risk-under 5%. But if you’re on insulin, glimepiride, glyburide, or repaglinide, your risk jumps to 15-40% annually. Sulfonylureas are especially tricky because they keep forcing your pancreas to release insulin, even when your blood sugar drops. That’s why many doctors now switch older patients from glyburide to glimepiride-it’s less likely to cause lows. If you’re on multiple medications, check for interactions. Beta-blockers for high blood pressure can hide the warning signs of low blood sugar, like a racing heart or shaking. You might not feel it coming until it’s too late.Understand the Three Levels of Hypoglycemia
The American Diabetes Association classifies lows into three levels. Level 1 is glucose below 70 mg/dL with symptoms. Level 2 is below 54 mg/dL-this is dangerous, even if you don’t feel anything. Level 3 is severe: you need help from someone else because you’re confused, unconscious, or having a seizure. Most people focus on Level 1, but Level 2 is the real red flag. If you hit Level 2 more than once a month, your treatment plan needs a serious rethink. Studies show that patients with repeated Level 2 events are 5 times more likely to have a severe low within the next year. Don’t wait for a crisis. Track your numbers. If you’re using a CGM, set alerts at 70 and 54 mg/dL. If you’re still finger-sticking, check before meals, at bedtime, and if you feel off-even if you think it’s just stress or fatigue.The 15-15 Rule (and Why Most People Get It Wrong)
When your blood sugar drops, you need fast-acting sugar. Not fruit, not candy bars, not honey straight from the jar. You need precisely 15 grams of pure glucose. That’s four glucose tablets, or 4 ounces of regular soda (not diet), or 1 tablespoon of sugar dissolved in water. Wait 15 minutes. Check again. If you’re still below 70, repeat. This is the 15-15 rule-and it works 89% of the time when done right. But here’s the problem: 63% of people use the wrong stuff. They grab a banana, thinking it’s healthy. Or they eat a whole chocolate bar, which spikes and crashes later. Or worse-they use sugar-free gum, which does nothing. Keep glucose tablets in your car, your purse, your desk drawer, and your bedside table. Glucagon kits (like Baqsimi nasal spray) are for emergencies when you can’t swallow. Keep one with you, and make sure someone close to you knows how to use it. Don’t wait until you’re unconscious to teach them.
Prevention Starts with Routine, Not Luck
You can’t just hope to avoid lows. You need structure. Start by logging everything: medication time, dose, what you ate, activity level, and your blood sugar reading. A simple notebook or app works. The Joslin Diabetes Center found that people who kept detailed logs reduced lows by over 50% in six months. Pay attention to patterns. Do you always drop after afternoon walks? Then eat 15 grams of carbs before you go. Do you crash at 3 a.m.? Talk to your doctor about adjusting your nighttime insulin. Alcohol is a silent trigger-it blocks your liver from releasing glucose. One drink can cause a low hours later, especially if you skip dinner. If you drink, always eat carbs with it. Exercise is another big one. A 30-minute walk can drop your sugar by 30-50 mg/dL. Adjust your insulin or eat extra carbs before or after. And don’t skip meals. A survey of 1,247 people found that 68% skipped meals because they were afraid of lows-and ended up having them anyway. Consistency beats perfection.Technology Can Be Your Best Ally
Continuous glucose monitors (CGMs) like Dexcom G7 or Freestyle Libre 3 are game-changers. They don’t just tell you your number-they show you the trend. Are you falling fast? You can act before you feel anything. Studies show CGMs cut severe lows by 48% and reduce time spent in hypoglycemia by 35%. But cost is a barrier. Medicare now covers CGMs for all insulin users, but out-of-pocket costs can still hit $1,200 a year. If you can’t afford one, start with a smart insulin pen. Pens like the InPen track your doses and times. You can see if you’re taking insulin too close to meals or if you’re overdosing at night. Even basic pattern recognition helps. If you notice your sugar drops every time you take glipizide at 8 a.m. and eat at 9:30 a.m., shift your medication to 7:30 a.m. Small changes add up.When to Call Your Doctor
If you’ve had two or more Level 2 lows in a month, or any Level 3 event, it’s time to revisit your treatment. Don’t wait for your next annual checkup. Ask for a medication review. Your doctor might switch you from a sulfonylurea to a GLP-1 agonist, reduce your insulin dose, or add a medication that lowers risk. If you have hypoglycemia unawareness-where you don’t feel the warning signs-you need a different approach. This affects 25% of type 1 patients after 20 years. You may need to aim for higher blood sugar targets temporarily (80-130 mg/dL) to retrain your body’s warning system. Your doctor might also recommend a CGM with predictive alerts or an automated insulin delivery system like Control-IQ. These systems pause insulin when your sugar is dropping. They’re not perfect, but they’ve been shown to reduce nighttime lows by over 3 hours per night.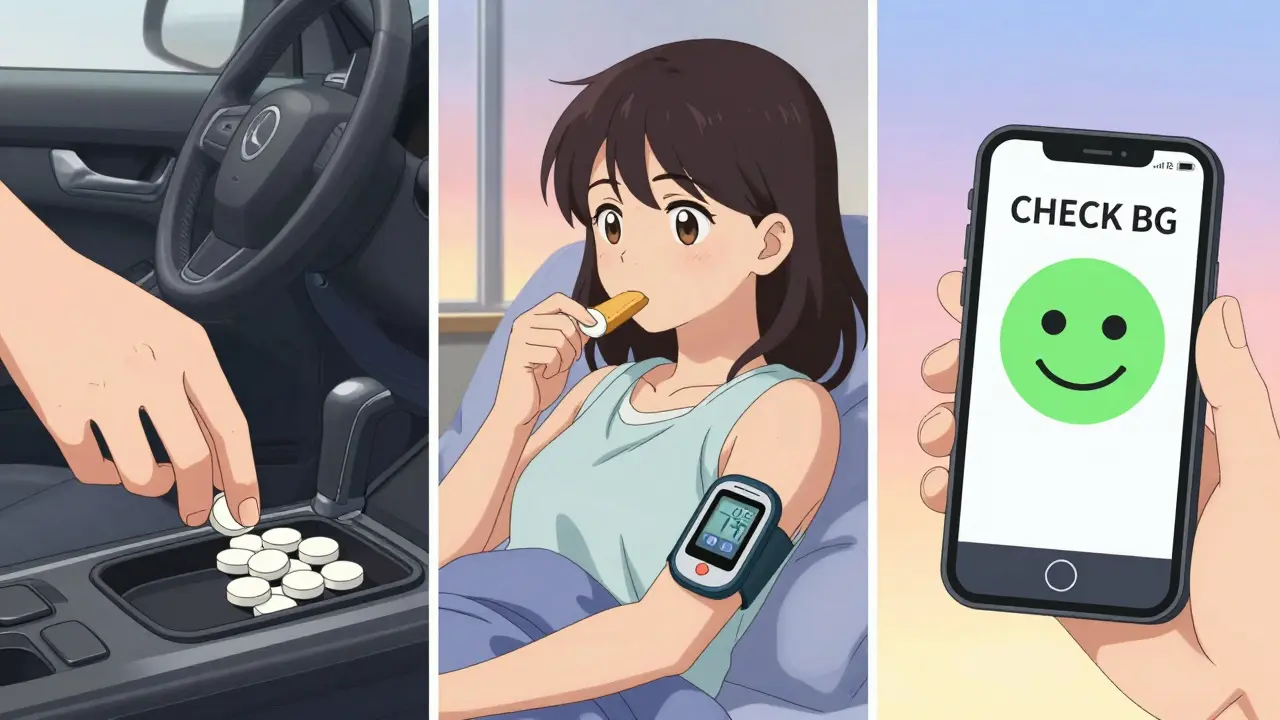
What Works in Real Life
People who manage this well don’t rely on willpower. They build systems. They keep a “hypo bag” in every room: glucose tabs, a glucagon kit, and a note saying what to do if they pass out. They set phone alarms for meals and bedtime checks. They teach their kids, partners, or coworkers how to use glucagon. One man in Melbourne told his local pharmacy to keep a spare glucagon kit behind the counter-just in case. Another woman started eating a small snack with protein and carbs before bed after she had three nighttime lows in two weeks. She hasn’t had one since. You don’t need to be perfect. You just need to be prepared. And consistent.What’s Coming Next
The future is getting smarter. New glucagon formulations like Zegalogue work in seconds, not minutes. AI-powered insulin pumps are learning your patterns and adjusting doses automatically. By 2030, most people on insulin will likely use closed-loop systems. But right now, the tools you have-glucose tablets, CGMs, careful logging-are enough. You don’t need the latest gadget to stay safe. You just need to know what to do, when to do it, and how to make it part of your daily life.Can metformin cause low blood sugar?
No, metformin alone very rarely causes hypoglycemia-less than 5% of users experience it. The risk only increases if metformin is combined with insulin or sulfonylureas. If you’re on metformin and having lows, talk to your doctor about your other medications.
What should I do if I pass out from low blood sugar?
If you pass out or can’t swallow, do NOT try to give food or drink. Use a glucagon injection or nasal spray (like Baqsimi or Gvoke) immediately. Call emergency services. Make sure family or coworkers know where your glucagon kit is and how to use it. Glucagon works even if you’re unconscious-it tells your liver to release stored sugar.
Is it safe to drive with diabetes and a risk of hypoglycemia?
Yes, but only if you check your blood sugar before driving and keep fast-acting carbs in the car. Never drive if your sugar is below 70 mg/dL. If you’ve had a severe low in the past 6 months or have hypoglycemia unawareness, talk to your doctor about restrictions. In Australia, you must report hypoglycemia episodes that affect your ability to drive safely to VicRoads.
Why do I get low blood sugar at night?
Nighttime lows often happen because your insulin dose is too high for your evening meal or activity level. Alcohol, skipping dinner, or exercising late can also trigger them. Check your blood sugar before bed. If it’s below 80 mg/dL, eat a small snack with protein and complex carbs. Consider using a CGM to catch drops early. Adjusting your long-acting insulin dose with your doctor can also help.
How do I know if I have hypoglycemia unawareness?
You may have it if you frequently have low blood sugar without feeling the usual symptoms like shaking, sweating, or hunger. This often happens after many years with diabetes, especially type 1. If you’ve had a severe low without warning, or if you’re surprised by low readings, talk to your doctor. You may need to aim for higher glucose targets for a few weeks to retrain your body’s warning system.
Next Steps: Your 7-Day Action Plan
Day 1: Check your current meds. List all diabetes drugs you take. Highlight any that carry high hypoglycemia risk (insulin, sulfonylureas, meglitinides).Day 2: Get glucose tablets. Buy a pack of 20 (14g each). Keep one in your wallet, car, and bedside drawer.
Day 3: Set up a simple log. Use your phone notes or a notebook. Record: date, time, blood sugar, meds taken, food eaten, activity.
Day 4: Talk to someone close to you. Show them your glucagon kit (if you have one) and explain what to do if you can’t respond.
Day 5: Review your last 10 blood sugar readings. Look for patterns-any lows after meals, exercise, or at night?
Day 6: Call your doctor. Ask: “Am I on the safest medication for my risk level?” and “Should I consider a CGM?”
Day 7: Set a phone alarm for 10 minutes before your next meal. Use it to check your blood sugar and prepare a snack if needed.
You don’t need to fix everything at once. Just start with one step. Then another. Low blood sugar is manageable-not inevitable.


Been using a CGM for 8 months now and honestly? Life-changing. I used to panic every time I felt a little off. Now I see the trend line dropping before I even get dizzy. No more 3 a.m. panic attacks. Just a quiet alert and a glucose tab. Seriously, if you're on insulin, get one. Even if you have to beg your insurance.