Melanoma is the deadliest form of skin cancer, but it’s also one of the most preventable. Unlike other skin cancers that grow slowly, melanoma can spread quickly if not caught early. The good news? When found in its earliest stage, more than 99% of people survive at least five years. When it spreads to other organs, that number drops to 35%. The difference between life and death often comes down to one thing: whether you caught it in time.
What Causes Melanoma?
Melanoma starts in melanocytes - the cells that give your skin its color. Most cases are caused by ultraviolet (UV) radiation from the sun or tanning beds. About 90% of melanomas are linked to UV exposure, according to the Cure Melanoma Foundation. That means most cases aren’t just bad luck - they’re preventable. People with fair skin, light eyes, or a history of sunburns are at higher risk. But melanoma doesn’t ignore darker skin. In fact, Black and Hispanic patients are more likely to be diagnosed at later stages because melanoma often shows up in unusual places - like under the nails, on the palms, or soles of the feet. This type, called acral lentiginous melanoma, makes up 2-8% of cases but is more common in people of color.How to Spot Melanoma: The ABCDE Rule
The ABCDE rule is the simplest way to check your skin for warning signs. You don’t need a doctor to use it. Just look at any mole or spot and ask:- A - Asymmetry: Does one half look different from the other?
- B - Border: Is the edge blurry, jagged, or uneven?
- C - Color: Does it have multiple shades - black, brown, red, white, or blue?
- D - Diameter: Is it larger than a pencil eraser (about 6mm)?
- E - Evolving: Has it changed in size, shape, color, or texture over weeks or months?
When to See a Dermatologist
You don’t need to wait for all five ABCDE signs to appear. If a spot looks odd, itchy, bleeds, or just doesn’t feel right - get it checked. High-risk people should see a dermatologist every 3 to 6 months. That includes anyone with:- More than 50 moles
- A family history of melanoma
- A past melanoma diagnosis
- Fair skin that burns easily
- History of severe sunburns
Prevention: It’s Not Just Sunscreen
Sunscreen is important, but it’s not enough. The CDC found that only 14% of high school students use sunscreen consistently. Cost is a big reason - 67% of low-income families say sunscreen is too expensive. Real prevention means a full strategy:- Wear UPF 50+ clothing and wide-brimmed hats
- Skip tanning beds - they raise melanoma risk by 58%
- Seek shade between 10 a.m. and 4 p.m.
- Check the UV index daily - the CDC is now integrating it into weather apps
- Apply broad-spectrum SPF 30+ every day, even when it’s cloudy
How Melanoma Is Diagnosed
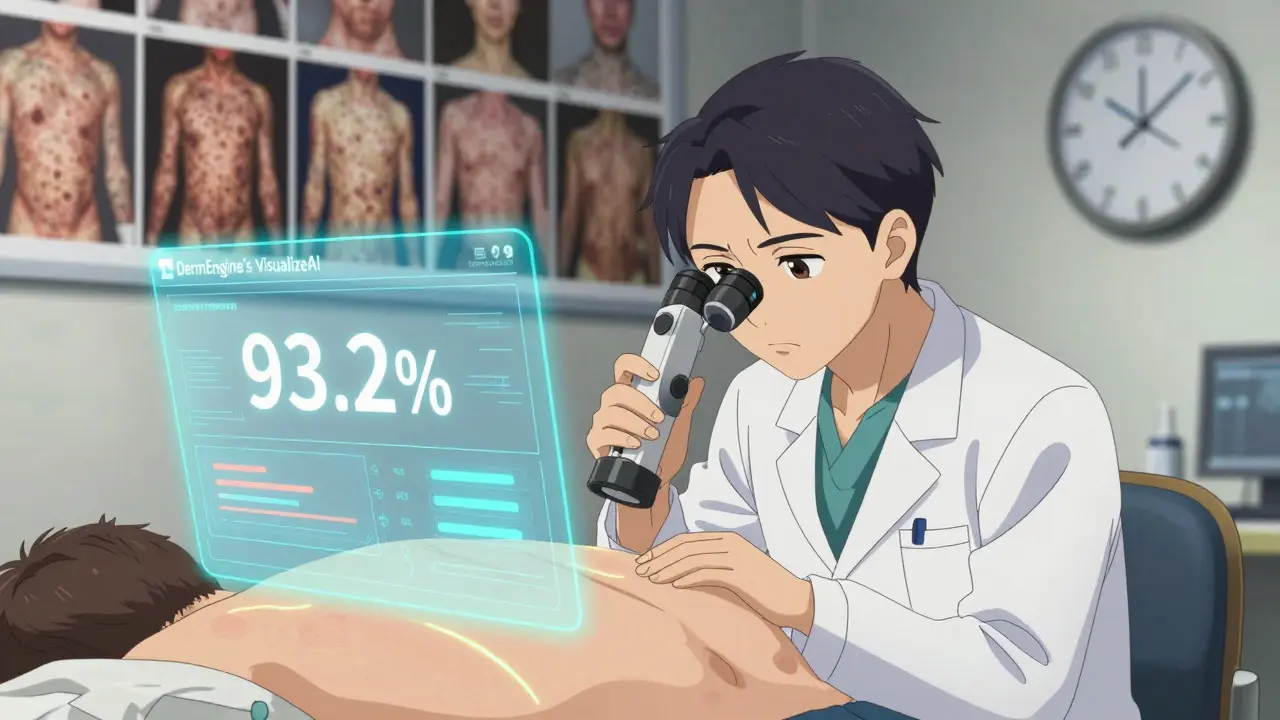
If a doctor suspects melanoma, they’ll likely use one or more tools:- Dermoscopy: A handheld magnifier with light that lets doctors see below the skin’s surface. It boosts accuracy from 65% to 90%.
- Total body photography: Takes 15-20 minutes and creates a full-body map of moles. Changes over time show warning signs.
- Reflectance confocal microscopy: A non-invasive imaging tool with 94% sensitivity - it can sometimes avoid biopsies.
- AI-assisted tools: In early 2025, the FDA approved DermEngine’s VisualizeAI, which correctly identified melanoma in 93.2% of cases across multiple clinics.
Stages of Melanoma and Treatment Options
Melanoma is staged from 0 to IV, based on thickness, spread, and whether it reached lymph nodes or organs.- Stage 0 (in situ): Confined to the top layer of skin. Treated with a simple excision - 0.5-1 cm margins. Survival rate: nearly 100%.
- Stage I-II: Deeper, but still local. Surgery with 1-2 cm margins. Sentinel lymph node biopsy (SLNB) is done if tumor is over 0.8 mm. Five-year survival: 97% for Stage IA.
- Stage III: Spread to nearby lymph nodes. Surgery plus adjuvant therapy - drugs like nivolumab, pembrolizumab, or ipilimumab. Costs $150,000-$200,000 per year.
- Stage IV: Spread to distant organs. Immunotherapy or targeted therapy. The combo of nivolumab and ipilimumab (CheckMate 067 trial) gave 52% of patients a 5-year survival rate.
The Cost of Treatment and Access Gaps
Melanoma treatment costs $3.4 billion annually in the U.S. But the real issue isn’t just price - it’s access. A 2024 report showed that 23.7 million Americans live more than 50 miles from an NCI-designated cancer center. In states like Mississippi, with just 1.2 dermatologists per 100,000 people, 22% of melanomas are diagnosed at late stages. In Massachusetts, with 7.8 dermatologists per 100,000, it’s only 14%. Patients on Reddit and patient forums report heartbreaking stories. One user, “MelanomaWarrior99,” paid $28,500 out-of-pocket for a single infusion of nivolumab - even with insurance. Another, “DJohnson_MD,” was misdiagnosed three times before being told their foot lesion was Stage III acral melanoma. New efforts are trying to close the gap. Walmart is piloting teledermatology kiosks in 150 clinics. The CDC is funding UV index alerts in weather apps - aiming to reach 120 million users by 2026.What’s New in 2025
The first half of 2025 brought two major breakthroughs:- Neoantigen vaccine (mRNA-4157/V940): Combined with pembrolizumab, it cut recurrence risk by 44% in high-risk Stage IIB-IV patients.
- AI dermoscopy (DermEngine’s VisualizeAI): FDA-approved with 93.2% accuracy - now being rolled out in clinics nationwide.
What You Can Do Today
You don’t need a medical degree to save your life. Here’s your action plan:- Check your skin every month. Use the ABCDE rule. Take a photo if you’re unsure.
- Protect yourself daily. Wear sunscreen, hats, and UV-blocking clothes - even on cloudy days.
- Know your risk. If you have many moles or a family history, schedule a dermatologist visit.
- Speak up. If a doctor dismisses a spot that looks wrong, ask for a biopsy.
- Help others. Share what you know. Melanoma doesn’t care about your income, skin tone, or age - but prevention does.
Can melanoma be prevented completely?
While you can’t eliminate all risk, up to 90% of melanomas are caused by UV exposure - meaning most cases are preventable. Using sunscreen daily, avoiding tanning beds, wearing protective clothing, and seeking shade during peak sun hours can reduce your risk dramatically. Regular skin checks also catch early changes before they become dangerous.
Is melanoma only a concern for people with fair skin?
No. While melanoma is more common in fair-skinned people, it’s often diagnosed later in people with darker skin. It tends to appear on less sun-exposed areas like the palms, soles, or under nails - and is more likely to be mistaken for a bruise or injury. Acral lentiginous melanoma, a type more common in Black and Asian populations, accounts for 2-8% of all cases. Everyone should check their entire body, not just sun-exposed areas.
How often should I get a professional skin exam?
If you’re at high risk - meaning you have over 50 moles, a family history of melanoma, or a past diagnosis - you should see a dermatologist every 3 to 6 months. For low-risk people, an annual check is enough. But monthly self-exams are critical for everyone, regardless of risk level. Don’t wait for a yearly visit to notice changes.
Do I need a biopsy if a mole looks suspicious?
Yes. Even advanced tools like dermoscopy or AI can’t replace a biopsy for a definitive diagnosis. If a dermatologist suspects melanoma, they’ll remove a small sample of the tissue and send it to a lab. This is the only way to confirm whether it’s cancer and how deep it has grown - which determines your treatment plan.
Can melanoma come back after treatment?
Yes, especially in Stage III and IV cases. That’s why follow-up care is essential - regular skin checks, imaging scans, and blood tests are often needed for years after treatment. New treatments like the mRNA-4157/V940 vaccine are showing promise in reducing recurrence risk by 44% when combined with immunotherapy. Staying vigilant after treatment is just as important as catching it early.


Man, I never realized how much melanoma hides in plain sight-especially under nails or on soles. I’ve got a dark spot on my pinky toe I’ve been ignoring since last summer. Guess I’m booking a derm appointment this week. Thanks for the wake-up call.