Every year, more than 100,000 people in the U.S. are diagnosed with invasive melanoma - the deadliest form of skin cancer. But here’s the truth: melanoma is one of the most preventable and treatable cancers if caught early. You don’t need to be a dermatologist to save your life. You just need to know what to look for, how to protect yourself, and what to do next if something feels off.
What Exactly Is Melanoma?
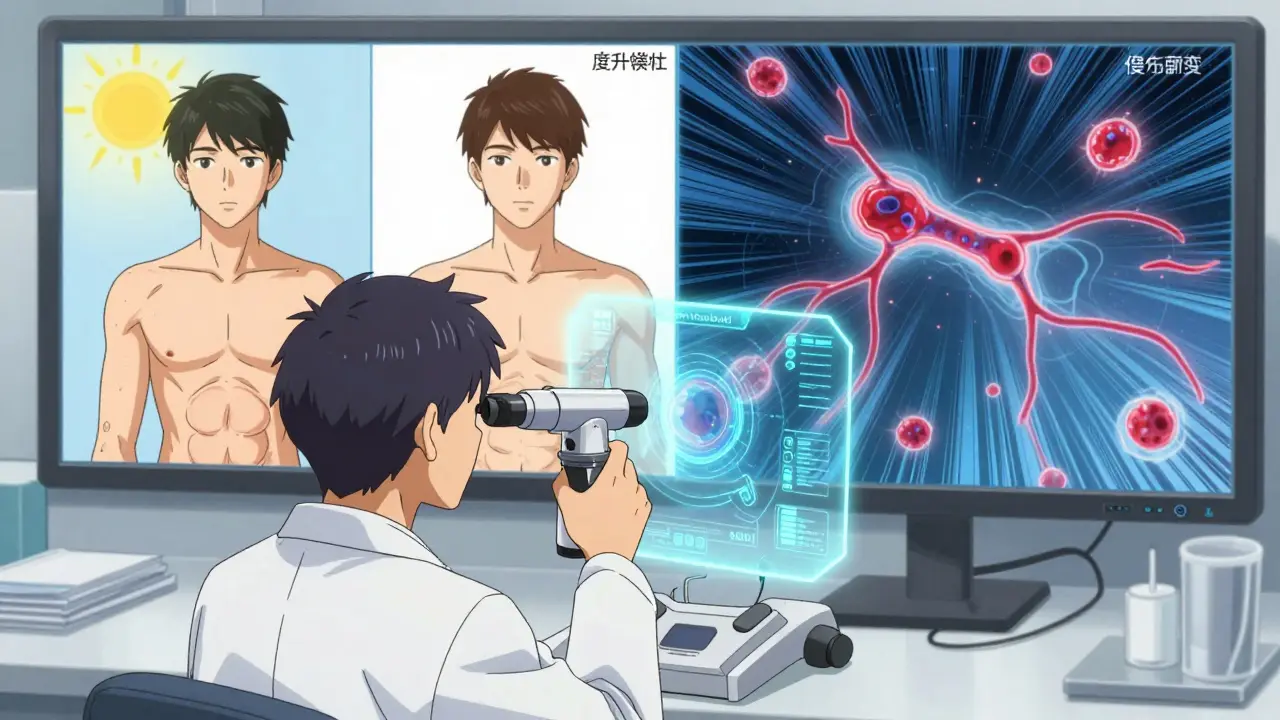
Melanoma starts in melanocytes - the cells that give your skin its color. While it makes up only about 1% of all skin cancers, it causes the vast majority of skin cancer deaths. That’s because it can spread fast if not caught in time. Unlike basal cell or squamous cell cancers, which usually stay on the surface, melanoma can dive deep into your skin and travel to lymph nodes or organs like the lungs or brain.
There are four main types:
- Superficial spreading melanoma (70% of cases) - starts as a flat, irregular mole that grows sideways before going deeper.
- Nodular melanoma (15-30%) - looks like a raised bump, often black or dark, and grows quickly.
- Lentigo maligna melanoma (10-15%) - usually found on sun-exposed areas like the face in older adults.
- Acral lentiginous melanoma (2-8%) - appears on palms, soles, or under nails. More common in people with darker skin and often missed because it doesn’t look like a typical mole.
It doesn’t matter if you have fair skin or dark skin. Melanoma can show up anywhere - even in places you never expose to the sun.
How to Spot Melanoma Early: The ABCDE Rule
You don’t need a fancy tool to catch melanoma. Your eyes and a mirror are enough. The ABCDE rule is still the gold standard for self-checks:
- A - Asymmetry: One half of the spot doesn’t match the other.
- B - Border: Edges are ragged, blurred, or uneven.
- C - Color: It has multiple shades - black, brown, red, white, or blue.
- D - Diameter: Larger than 6mm (about the size of a pencil eraser).
- E - Evolving: It’s changing in size, shape, color, or texture over weeks or months.
But here’s the catch: not all melanomas follow the rules. Some are tiny. Some are pink. Some don’t even look like moles - they might look like a bruise that won’t heal, a scab that keeps coming back, or a streak under your nail.
According to patient reports on the Melanoma Research Foundation forum, 78% of people found their own melanoma during a self-exam. That’s not luck. It’s awareness. Make time once a month - after a shower, when your skin is clean and well-lit - to check your whole body. Use a hand mirror for hard-to-see spots. Take photos if you want to track changes over time.
Who’s at Risk - And Why It’s Not Just Fair-Skinned People
Most people think melanoma only affects those with pale skin, freckles, and a history of sunburns. That’s partly true. But here’s what’s often ignored:
- People with 50 or more moles are at higher risk.
- If a parent, sibling, or child had melanoma, your risk doubles.
- Those with weakened immune systems - from organ transplants, HIV, or certain medications - are more vulnerable.
- And here’s the big one: people with darker skin are more likely to die from melanoma. Why? Because it’s often diagnosed later. Acral lentiginous melanoma, which shows up on the soles of feet or under nails, is more common in Black, Asian, and Hispanic populations. But doctors - and patients - often mistake it for a bruise or injury.
One patient on Reddit, 'DJohnson_MD', described how doctors dismissed a dark line under his toenail as a bruise for over a year. By the time it was biopsied, it was Stage III. He survived - but barely.
Age matters too. The average age at diagnosis is 65, but melanoma is one of the top cancers in people under 30. Young adults think they’re invincible. They don’t realize that indoor tanning - even once a month - increases melanoma risk by 58%.

Prevention: It’s Not Just About Sunscreen
90% of melanomas are linked to UV radiation. That’s the good news - because UV exposure is something you can control.
Sunscreen alone isn’t enough. You need a full strategy:
- Wear UPF 50+ clothing - hats, long sleeves, and UV-blocking sunglasses. A regular T-shirt only blocks about 5 UV rays. A UPF-rated shirt blocks over 98%.
- Avoid the sun between 10 a.m. and 4 p.m. That’s when UV rays are strongest.
- Never use tanning beds. The FDA classifies them as carcinogenic - same as asbestos and tobacco.
- Use broad-spectrum SPF 30+ daily, even on cloudy days. UV rays penetrate clouds. And don’t forget your ears, neck, lips, and feet.
- Check the UV index. New apps like QSun’s UV Index now integrate with weather forecasts. When the index is 6 or higher, take extra precautions.
Here’s the kicker: every $1 spent on UV protection saves $3.50 in future treatment costs. Yet, only 14.3% of high school students use sunscreen regularly. Cost is a barrier for 67% of low-income families. That’s why new CDC programs are rolling out UV index alerts in weather apps - aiming to reach 120 million people by 2026.
Detection Tools: Beyond the Mirror
If you’re high-risk - lots of moles, family history, past sunburns - you need more than self-checks.
- Dermoscopy: A dermatologist uses a handheld magnifier with a light to look at moles in detail. It raises diagnostic accuracy from 65% to 90%.
- Total body photography: A full-body scan takes 15-20 minutes. It creates a digital map of your moles so changes can be tracked over time. Systems like FotoFinder are used in clinics across the U.S.
- Reflectance confocal microscopy: A non-invasive imaging tool that lets doctors see skin layers without a biopsy. It’s 94% sensitive in spotting melanoma.
- AI-assisted tools: In early 2025, the FDA approved DermEngine’s VisualizeAI - an AI tool that analyzes dermoscopy images with 93.2% accuracy. It’s now being used in clinics to reduce missed diagnoses.
Teledermatology is growing fast. About 61% of dermatology practices now offer virtual visits. But it’s not perfect. Studies show teledermatology is 87% accurate - compared to 92% for in-person exams. Still, for people in rural areas where dermatologists are scarce (like in Mississippi, with only 1.2 per 100,000 people), it’s life-saving.
Treatment: What Happens After Diagnosis
Treatment depends entirely on how far the melanoma has spread.
- Stage 0 (in situ): The cancer is only in the top layer of skin. Surgery with a small margin (0.5-1 cm) is usually enough. Cure rate: nearly 100%.
- Stage I-II: The tumor is deeper but hasn’t spread. Surgery with wider margins (1-2 cm) is done, often with a sentinel lymph node biopsy to check if it’s moved. If caught at Stage IA, the 5-year survival rate is 97%.
- Stage III: Cancer has reached nearby lymph nodes. Surgery is followed by adjuvant therapy - drugs like nivolumab, pembrolizumab, or ipilimumab. These boost your immune system to fight leftover cancer cells. Cost? $150,000-$200,000 per year.
- Stage IV: The cancer has spread to distant organs. This is where things get complex. Two main options:
Immunotherapy: Drugs like nivolumab + ipilimumab. They don’t kill cancer directly - they teach your immune system to recognize and attack it. In the CheckMate 067 trial, 52% of Stage IV patients were still alive after five years. Side effects? About 14% had serious reactions.
Targeted therapy: For patients with BRAF mutations (about half of melanomas), drugs like dabrafenib + trametinib can shrink tumors fast. Median survival is 34 months. But side effects are harsh - 57% have serious reactions like fever, rash, or liver problems.
Doctors now test all Stage IIB-IV patients for BRAF, NRAS, KIT, and NF1 mutations. This isn’t optional - it’s standard. Your treatment path depends on your genetic profile.
The Hidden Crisis: Cost and Access
While survival rates have improved, access hasn’t.
One Reddit user, 'MelanomaWarrior99', shared that even with insurance, a single dose of nivolumab cost him $28,500 out-of-pocket. That’s not rare. Medicare spends $1.8 billion annually on melanoma treatment - but only $0.02 per person is spent on prevention.
There are also “treatment deserts.” In rural areas, 23.7 million Americans live more than 50 miles from a cancer center that offers advanced melanoma care. Meanwhile, academic centers perform 87% of complex surgeries. That means if you’re poor, live far away, or can’t take time off work - your odds drop.
And it’s not just about money. The average wait for a dermatology appointment is 28.7 days nationwide. In rural areas? Up to 63 days. That’s enough time for a small mole to turn dangerous.
What’s Next? The Future of Melanoma Care
In early 2025, the FDA approved two breakthroughs:
- mRNA-4157/V940: A personalized vaccine that trains your immune system to target your specific melanoma. When combined with pembrolizumab, it cut recurrence risk by 44% in Stage IIB-IV patients.
- DermEngine’s VisualizeAI: An AI tool that helps doctors spot melanomas faster and more accurately - especially in early stages.
By 2040, experts believe melanoma deaths could drop by 50% - if we focus on prevention and equity. But right now, progress is uneven. Wealthy, urban patients are living longer. Rural and low-income patients are falling behind.
That’s why new pilot programs are launching: teledermatology kiosks in 150 Walmart clinics, UV index alerts on weather apps, and free skin checks in community centers. These aren’t just nice ideas - they’re survival tools.
What You Should Do Right Now
You don’t need to wait for symptoms. Here’s your action plan:
- Do a full-body skin check once a month. Use a mirror. Take photos.
- Know your ABCDEs. If something changes - even slightly - see a dermatologist.
- Wear sunscreen daily. Wear UPF clothing. Avoid tanning beds - period.
- If you’re high-risk (many moles, family history, dark skin), get a professional exam every 3-6 months.
- If you’re uninsured or underinsured, look for free skin cancer screenings. Many dermatology societies offer them - especially in May, during Skin Cancer Awareness Month.
Early detection isn’t just about living longer. It’s about avoiding chemotherapy, avoiding surgery, avoiding debt. It’s about being here for your kids, your parents, your future.
One person wrote on a patient forum: “My 99.6% survival odds beat the 35% my oncologist showed me for late-stage cases.”
That’s the difference between catching it early - and not.


Wow, this is one of those posts that makes you pause and actually look at your own skin. I never realized how much melanoma can hide in plain sight-like under nails or on the soles of feet. I’m from India, and we’re often told we’re ‘protected’ because of darker skin, but that’s a dangerous myth. My uncle had a spot on his heel for years-thought it was a bruise from walking barefoot. Turned out Stage III. Don’t let ‘it doesn’t look like cancer’ fool you. Check your feet. Seriously.
Also, the part about UV index apps? I just downloaded QSun. Best decision I made this year. Now I check it before stepping out, even on cloudy days. Who knew weather apps could save lives?