Nudge Theory: How Small Changes Influence Health Decisions
When you think about changing your health habits, you probably imagine willpower, discipline, or a big lifestyle overhaul. But what if the best way to get people to take their meds, eat better, or move more isn’t through lectures or guilt—but through quiet, smart design? That’s the heart of nudge theory, a concept from behavioral economics that uses subtle environmental cues to guide people toward better decisions without restricting freedom of choice. Also known as choice architecture, it’s not about forcing change—it’s about making the right choice the easiest one.
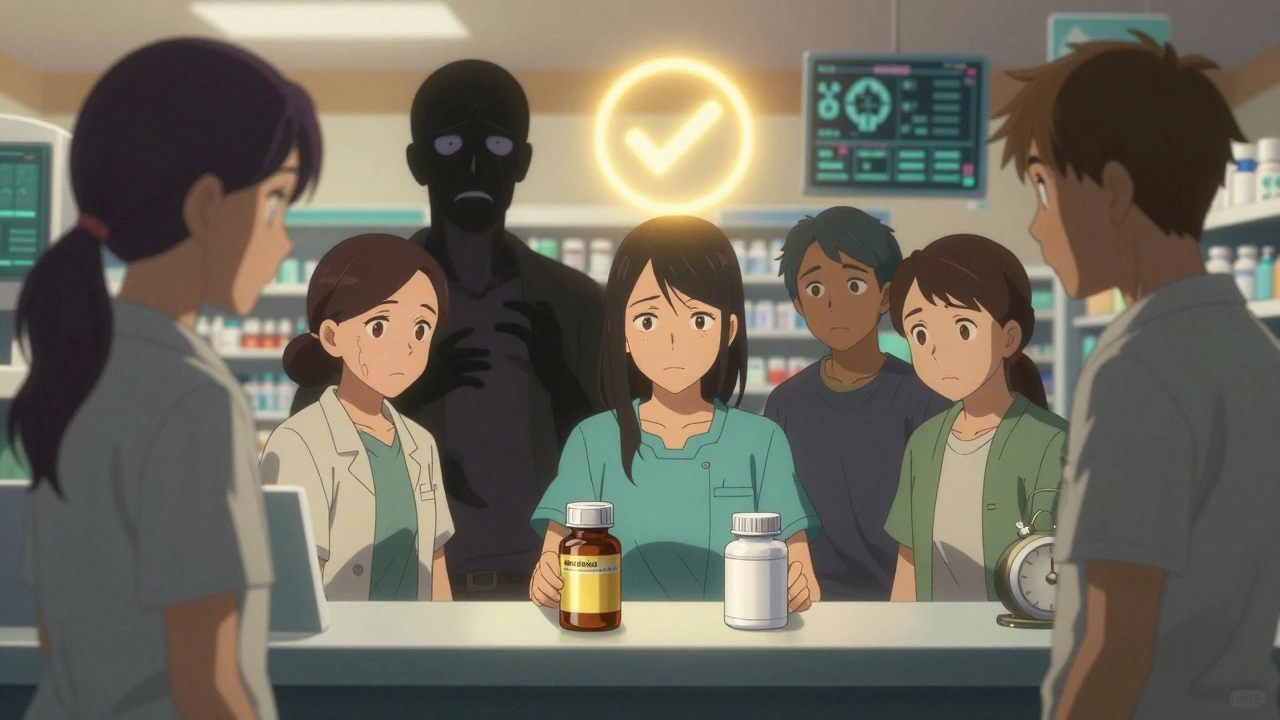
Nudge theory works because humans aren’t rational calculators. We forget pills, we grab the snack within arm’s reach, we delay doctor visits because the system feels too complicated. But when pharmacies put daily pill organizers next to coffee makers, when hospitals send text reminders timed to when people are most awake, or when healthy foods are placed at eye level in the clinic cafeteria—those are nudges. They don’t shout. They don’t punish. They just make the better option more visible, more convenient, or more normal. And studies show they work. One trial found that simply moving statins from the back shelf to the front counter of a pharmacy increased adherence by 27%. Another showed that patients who received a text message saying "Your next dose is due tomorrow" were twice as likely to take it as those who didn’t.
This isn’t just theory—it’s being used in real clinics, pharmacies, and even by insurers. Think about how medication adherence, the challenge of taking drugs exactly as prescribed is tackled in the posts below. Many of them don’t just explain side effects or risks—they show how small design changes can fix big problems. A pill bottle with a built-in timer. A monthly refill alert tied to your calendar. A doctor who asks, "What’s stopping you from taking this?" instead of "Why didn’t you take it?" These are all nudges. And they’re backed by data from real patients, not just lab studies.
It’s also why public health interventions, system-level efforts to improve population health are shifting from education campaigns to environmental tweaks. Instead of telling people to eat less sugar, some hospitals now remove sugary drinks from vending machines entirely. Instead of begging people to get flu shots, clinics offer them at the checkout counter. These aren’t tricks—they’re smart defaults. And they work better than posters, pamphlets, or even expensive apps.
What you’ll find in the posts below isn’t a list of abstract ideas. It’s a collection of real, practical stories about how small changes—like where a pill is stored, when a reminder pops up, or how a doctor frames a choice—can make a huge difference in how people manage chronic conditions, avoid dangerous interactions, and stick with treatments. You’ll see how nudge theory shows up in medication storage tips, in the way generics are presented to save money, in how side effects are discussed without scaring people off, and even in how pharmacies help patients switch from brand to generic without confusion. None of these rely on yelling or shame. They rely on understanding how people actually behave—and then designing around it.
Behavioral Economics: Why Patients Choose Certain Drugs Over Others
Behavioral economics explains why patients often choose expensive, familiar drugs over cheaper alternatives-driven by fear, habit, and cognitive biases. Learn how psychology, not just price, shapes medication decisions.
More Detail