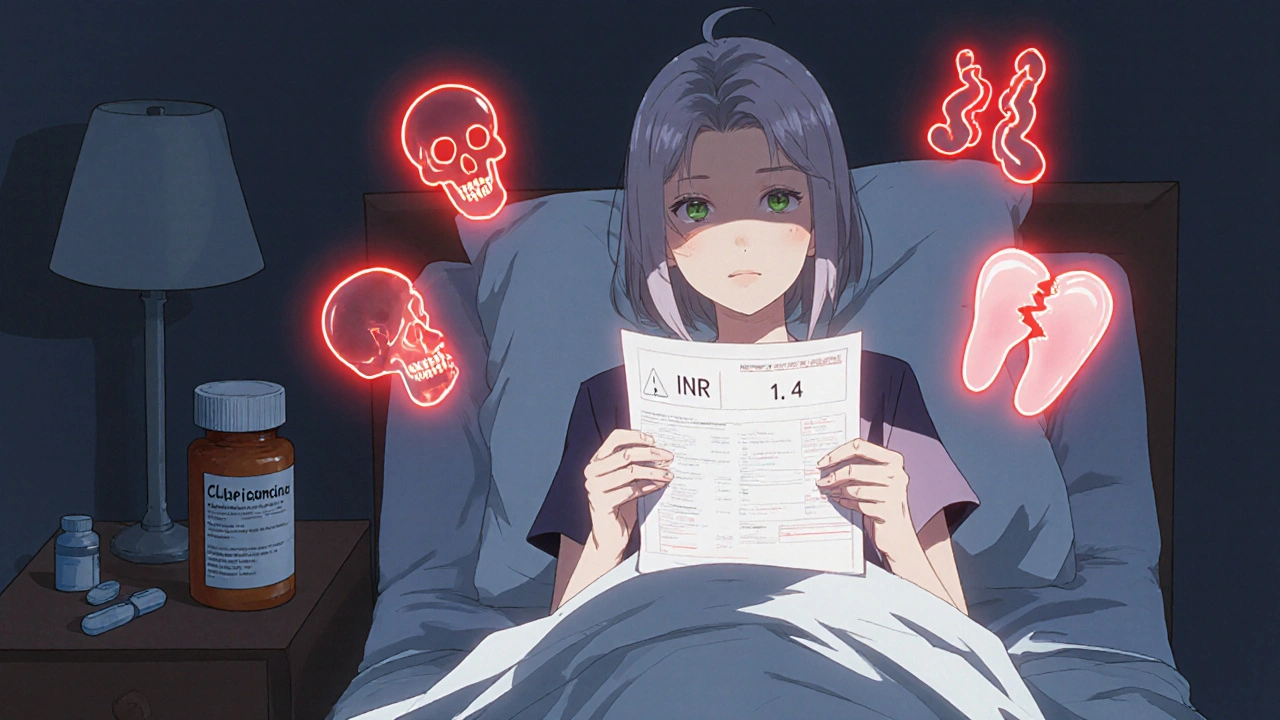
Warfarin Bleeding Risk: What You Need to Know Before Taking It
When you take warfarin, a blood thinner used to prevent clots in people with atrial fibrillation, artificial heart valves, or deep vein thrombosis. Also known as Coumadin, it works by blocking vitamin K, which your body needs to make clotting proteins. But this same mechanism is why warfarin bleeding risk is so serious—it doesn’t just stop bad clots, it can turn a small cut into a dangerous situation.
Warfarin doesn’t work the same for everyone. Your risk of bleeding depends on things like age, kidney function, diet, and other meds you’re taking. A simple change—like eating more kale or starting an antibiotic—can throw your INR (the test that measures how long your blood takes to clot) out of range. That’s why regular blood tests aren’t optional. If your INR is too high, even a bump on the head could lead to internal bleeding. If it’s too low, you’re not protected from stroke or pulmonary embolism. It’s a tightrope walk, and there’s no room for guesswork.
Some people think warfarin is outdated because newer blood thinners exist, but that’s not always true. For patients with mechanical heart valves, warfarin is still the gold standard. For others, it’s the only option their insurance covers. The key isn’t avoiding warfarin—it’s managing it right. That means knowing the warning signs: unusual bruising, pink or red urine, nosebleeds that won’t stop, headaches that feel different, or abdominal pain. These aren’t side effects you should ignore. And if you’re on warfarin, you need to tell every doctor, dentist, and pharmacist before any procedure, even a simple tooth extraction.
Many of the posts in this collection focus on how medications interact, how to track your treatments, and how to spot hidden risks. You’ll find guides on keeping a personal medication list, understanding drug labeling, and avoiding dangerous combinations—all things that matter when you’re on warfarin. You’ll also see how other drugs like antibiotics or pain relievers can quietly increase your bleeding risk. This isn’t theoretical. People end up in the ER because they took ibuprofen with warfarin and didn’t realize it was a problem. Or they skipped their INR test because they felt fine—and then fell and couldn’t stop bleeding.
There’s no magic fix. But with the right knowledge, you can take warfarin safely for years. It’s not about fear. It’s about awareness. You don’t need to be a medical expert—you just need to know what to watch for, when to call your doctor, and how to keep your treatment on track. The articles below give you real, practical tools to do exactly that.
Warfarin and Antibiotics: How Common Antibiotics Can Spike Your INR Risk
Warfarin and certain antibiotics can dangerously raise INR levels, increasing bleeding risk. Learn which antibiotics are most risky, how to monitor your INR, and what to do if your levels spike.
More Detail