Antibiotic Effects on INR: What You Need to Know
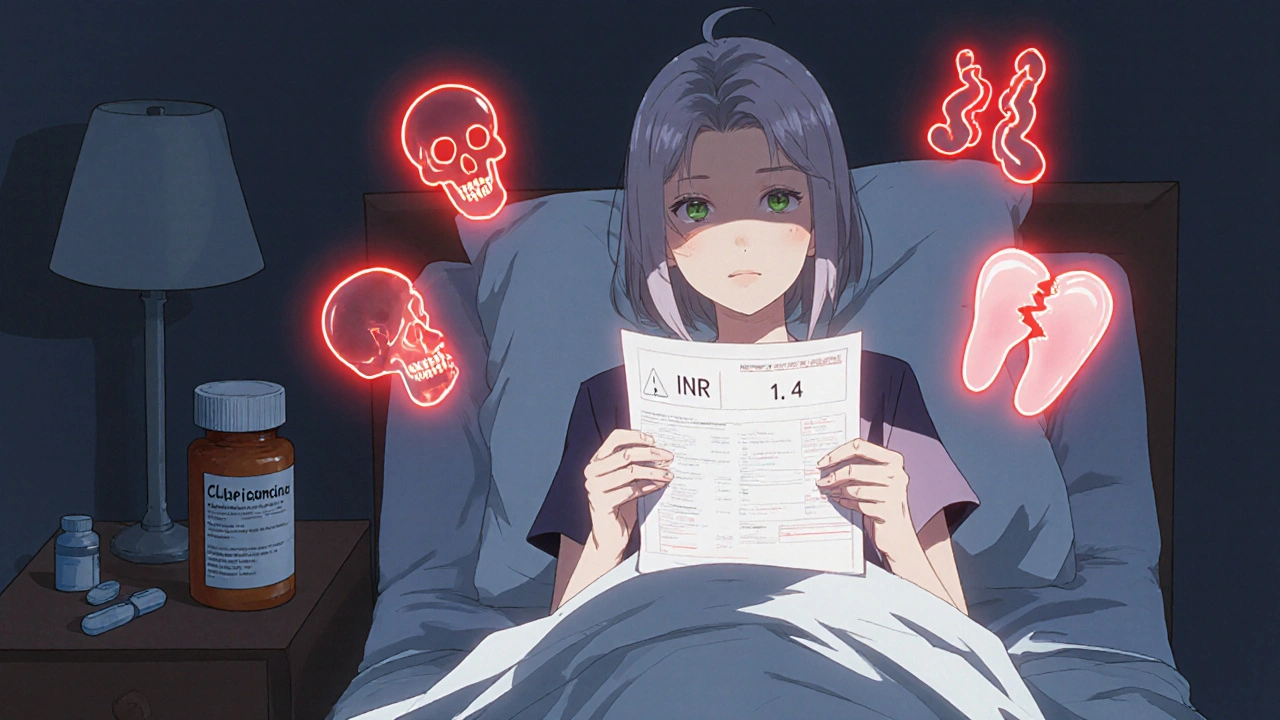
When you're taking warfarin, a blood thinner used to prevent clots by slowing down clotting factors. Also known as Coumadin, it requires regular monitoring of your INR, a standardized measure of how long it takes your blood to clot. This number tells your doctor if your dose is safe—too low, and you risk clots; too high, and you could bleed internally. Now, add an antibiotic, a drug that kills or stops bacteria from growing. Some antibiotics don’t just target infection—they also interfere with how warfarin works in your body. That’s where things get risky.
Not all antibiotics affect INR the same way. Antibiotic effects on INR are most common with fluoroquinolones like ciprofloxacin and levofloxacin, and with sulfonamides like trimethoprim-sulfamethoxazole. These drugs slow down how fast your liver breaks down warfarin, causing it to build up in your blood. That pushes your INR higher, sometimes dangerously so. Other antibiotics, like amoxicillin or azithromycin, usually don’t touch INR at all. But here’s the catch: even if a drug is "safe," your body might react differently. Age, liver function, diet, and other meds all play a role. A 72-year-old on warfarin for atrial fibrillation might see their INR jump from 2.5 to 6.0 after just three days of ciprofloxacin. That’s not a coincidence—it’s a known interaction backed by real patient data.
What should you do? If you’re on warfarin and your doctor prescribes an antibiotic, don’t assume it’s fine. Ask: "Will this change my INR?" and "Do I need a blood test sooner than usual?" Many patients don’t realize they should check their INR within 3 to 5 days after starting a new antibiotic. Waiting until your next scheduled test could be too late. Keep your medication list updated—include every antibiotic, even over-the-counter ones like bismuth subsalicylate (Pepto-Bismol), which can also affect INR. And never stop or change your warfarin dose on your own, even if you feel fine. Bleeding risks don’t always come with warning signs.
The posts below cover real-world cases and comparisons you won’t find in generic pamphlets. You’ll see how cefaclor and tinidazole interact with other drugs, how patients track their meds to avoid surprises, and what to do when a recall hits your prescription. These aren’t theory pieces—they’re tools for people who live with blood thinners and need to stay safe while treating infections.
Warfarin and Antibiotics: How Common Antibiotics Can Spike Your INR Risk
Warfarin and certain antibiotics can dangerously raise INR levels, increasing bleeding risk. Learn which antibiotics are most risky, how to monitor your INR, and what to do if your levels spike.
More Detail