Immunosuppressants: What They Are, How They Work, and What You Need to Know
When your immune system turns against your own body—or threatens a transplanted organ—immunosuppressants, drugs that lower the body’s immune response to prevent damage or rejection. Also known as anti-rejection drugs, they’re not optional for people with transplanted kidneys, hearts, or livers, and they’re critical for managing conditions like lupus, rheumatoid arthritis, and Crohn’s disease. These aren’t painkillers or antibiotics. They don’t cure anything. They simply quiet down an overactive defense system so it doesn’t destroy healthy tissue. But that quieting comes with consequences.
Immunosuppressants work by targeting specific parts of your immune system. Some block signals between immune cells, others kill off aggressive white blood cells, and a few stop the body from making new ones. That’s why they’re often paired with other meds—like corticosteroids, powerful anti-inflammatory drugs often used short-term to kickstart immune control—or combined with calcineurin inhibitors, a class of drugs including tacrolimus and cyclosporine that prevent T-cells from activating. But because these drugs weaken your body’s natural defenses, you’re more vulnerable to infections, and some carry long-term risks like kidney damage, high blood pressure, or even certain cancers. That’s why monitoring is non-negotiable: regular blood tests, tracking symptoms like fever or unusual fatigue, and knowing which drug interactions, especially with common antibiotics or antifungals, can spike toxicity levels are part of daily life for anyone on these meds.
You’ll also hear about side effects like tremors, headaches, or swollen gums—but the real challenge isn’t the physical stuff. It’s sticking with the regimen. Missing a dose, even once, can trigger rejection or a flare-up. That’s why adherence is so tightly linked to outcomes. Many people stop taking their meds because of cost, side effects, or just feeling fine. But feeling fine is exactly why you can’t stop. The drugs aren’t treating symptoms—they’re preventing a silent, potentially deadly process from restarting.
Below, you’ll find real-world guides on managing these drugs safely: how to spot dangerous interactions, what to do when side effects hit, how generics compare to brand names, and why some people need to be extra careful switching medications. These aren’t theoretical discussions—they’re based on what patients actually face every day. Whether you’re on immunosuppressants yourself, caring for someone who is, or just trying to understand why these drugs are so tightly controlled, this collection gives you the facts you need to stay safe and informed.
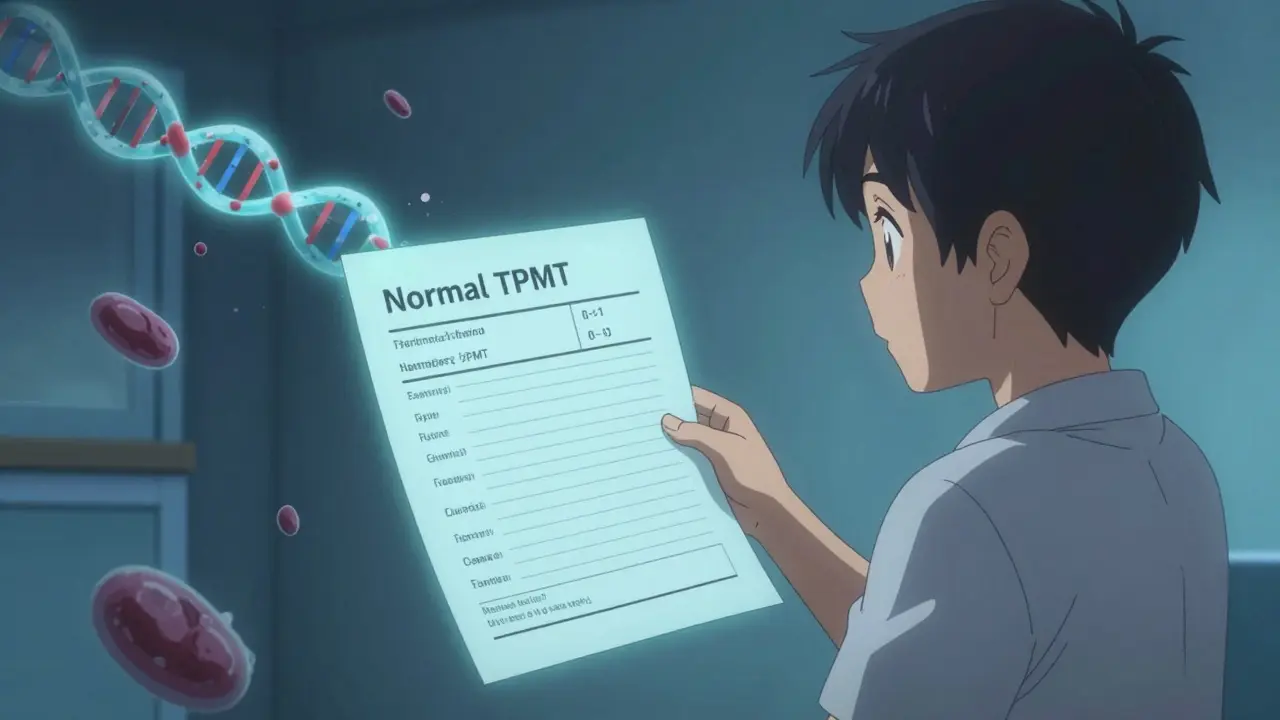
Azathioprine and TPMT Testing: How Genetic Screening Prevents Life-Threatening Side Effects
Azathioprine is a cost-effective immunosuppressant, but it can cause life-threatening blood cell damage in people with genetic enzyme deficiencies. TPMT and NUDT15 testing before starting the drug can prevent severe side effects like myelosuppression and liver toxicity.
More Detail
Grapefruit and Immunosuppressants: What You Need to Know Before You Eat It
Grapefruit can dangerously raise levels of immunosuppressants like cyclosporine and tacrolimus, leading to kidney damage, infections, or organ rejection. Even one glass can cause toxic effects lasting up to 72 hours.
More Detail